Factors Associated With Decision to Treat or Not to Treat Helicobacter pylori Infection in Children: Data From the EuroPedHp Registry
Abstract
Background
European and North-American guidelines on management of H. pylori infection in children provide the option not to treat even if the infection is endoscopically confirmed. We used data from the EuroPedHp Registry to identify factors associated with therapy decisions.
Methods
We included treatment-naïve patients reported between 2017 and 2020 from 30 centers in 17 European countries. Multivariable logistic regression identified factors including comorbidities within and outside the gastrointestinal (GI) tract influencing the decision for or against therapy.
Results
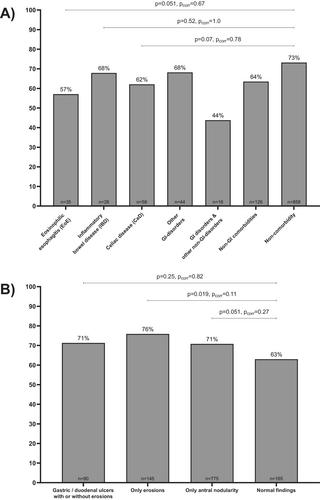
Of 1165 patients (52% females, median age 12.8), 28% (321/1165) reported any alarm symptom, 26% (307/1165) comorbidities, and 16% (192/1165) did not receive eradication treatment. Therapy was initiated less often in children having any GI comorbidity (57%, n = 181), particularly in those with eosinophilic esophagitis (60%, n = 35), inflammatory bowel disease (54%, n = 28), and celiac disease (43%, n = 58), compared to those with non-GI (86%, n = 126) or no comorbidity (89%, n = 858), despite similar frequencies of alarm and non-alarm symptoms, ulcers, erosions, and nodular gastritis. Patients with GI and without comorbidities remained more likely untreated in high versus low H. pylori prevalence countries (p < 0.0001). In children without comorbidities, factors favoring therapy included older age, being overweight, having symptoms, erosions, antral nodularity, and available antibiotic susceptibility results.
Conclusion
In this cohort, H. pylori-infected children with GI comorbidities compared to no comorbidity showed 75% reduced chance of receiving eradication therapy. We found no evidence supporting different management strategies in infected patients with GI comorbidities compared to all pediatric patients with endoscopically proven H. pylori infection.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


