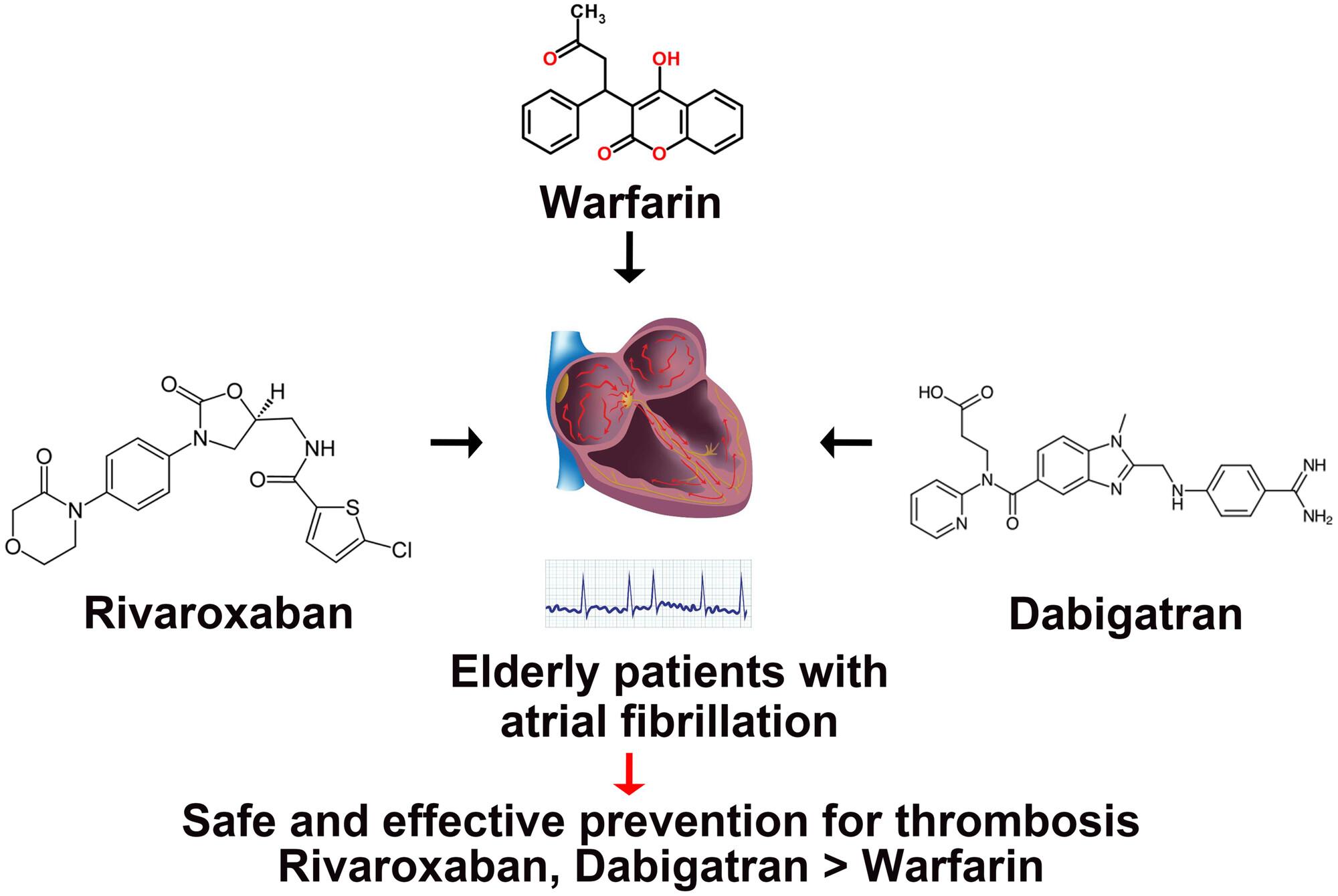
Application Value and Safety Analysis of Warfarin, Rivaroxaban, and Dabigatran Ester in Elderly Patients With Atrial Fibrillation
Abstract
Background
This study aimed to evaluate the application value and safety of Warfarin, Rivaroxaban, and Dabigatran in elderly patients with atrial fibrillation.
Methods
A total of 180 elderly patients with atrial fibrillation admitted to our hospital were retrospectively analyzed. According to their anticoagulant treatment regimen, patients were divided into three groups: Warfarin (57 cases), Rivaroxaban (61 cases), and Dabigatran (62 cases). General demographic information was collected, and coagulation function indicators—including fibrinogen (FIB), thrombin time (PT), activated partial thrombin time (APTT), and D-dimer (D-D)—as well as liver function indexes—including total bilirubin (TbiL), alkaline phosphatase (ALP), aspartate aminotransferase (AST), and alanine transferase (ALT)—were compared before and after 4 weeks of treatment.
Results
There were no significant differences in demographic characteristics such as gender, age, body mass index, or disease course among the three groups. The total effective rate in the Warfarin group (84.21%) was significantly lower than in the Rivaroxaban (98.36%) and Dabigatran (96.77%) groups (p < 0.05). However, there was no significant difference in the total effective rate between the Rivaroxaban and Dabigatran groups (p > 0.05). Additionally, no significant differences were found in the effects of the three drugs on coagulation function, liver function, or the incidence of bleeding (p = 0.052).
Conclusion
Warfarin, Rivaroxaban, and Dabigatran can effectively prevent thrombosis in elderly patients with atrial fibrillation, with Rivaroxaban and Dabigatran showing superior effectiveness. All three drugs demonstrated similar low rates of bleeding events and had no significant impact on coagulation and liver function.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


