Novel combined echocardiographic score comprising prognostically validated measures of left ventricular size and function to predict long-term survival following myocardial infarction: A proposal to improve risk stratification
Abstract
Background
While left ventricular ejection fraction (LVEF) is the primary variable utilized for prognosis following myocardial infarction (MI), it is relatively indiscriminate for survival in patients with mildly reduced (> 40%) or preserved LVEF (> 50%). Improving risk stratification in patients with mildly reduced or preserved LVEF remains an unmet need, and could be achieved by using a combination approach using prognostically validated measures of left-ventricular (LV) size, geometry, and function.
Aims
The aim of this study was to compare the prognostic utility of a Combined Echo-Score for predicting all-cause (ACM) and cardiac mortality (CM) following MI to LVEF alone, including the sub-groups with LVEF > 40% and LVEF > 50%.
Methods
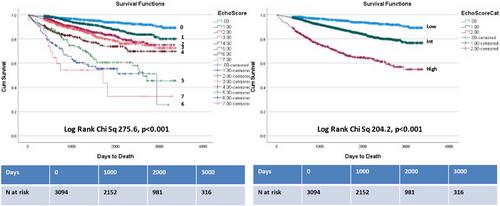
Retrospective data on 3094 consecutive patients with MI from 2013 to 2021 who had inpatient echocardiography were included, including both patients with ST-elevation MI (n = 869 [28.1%]) and non-ST-elevation MI (n = 2225 [71.9%]). Echo-Score consisted of LVEF < 40% (2 points) or LVEF < 50% (1 point), and 1 point each for left atrial volume index > 34 mL/m2, septal E/eʹ > 15, abnormal LV mass-index, tricuspid regurgitation velocity > 2.8 m/s, and abnormal LV end-systolic volume-index. Simple addition was used to derive a score out of 7.
Results
At a median follow-up of 4.5 years there were 445 deaths (130 cardiac deaths). On Cox proportional-hazards multivariable analysis incorporating significant clinical and echocardiographic predictors, Echo-Score was an independent predictor of both ACM (HR 1.34, p < .001) and CM (HR 1.59, p < .001). Inter-model comparisons of model 𝛘2, Harrel's C and Somer's D, and Receiver operating curves confirmed the superior prognostic value of Echo-Score for both endpoints compared to LVEF. In the subgroups with LVEF > 40% and LVEF > 50%, Echo-Score was similarly superior to LVEF for predicting ACM and CM.
Conclusions
An Echo-Score composed of prognostically validated LV parameters is superior to LVEF alone for predicting survival in patients with MI, including the subgroups with mildly reduced and preserved LVEF. This could lead to improved patient risk stratification, better-targeted therapies, and potentially more efficient use of device therapies. Further studies should be considered to define the benefit of further investigation and treatment in high-risk subgroups.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


