Fatal meningoencephalitis associated with Ebola virus persistence in two survivors of Ebola virus disease in the Democratic Republic of the Congo: a case report study
IF 20.4
1区 生物学
Q1 INFECTIOUS DISEASES
引用次数: 0
Abstract
Background
During the 2018–20 Ebola virus disease outbreak in the Democratic Republic of the Congo, thousands of patients received unprecedented vaccination, monoclonal antibody (mAb) therapy, or both, leading to a large number of survivors. We aimed to report the clinical, virological, viral genomic, and immunological features of two previously vaccinated and mAb-treated survivors of Ebola virus disease in the Democratic Republic of the Congo who developed second episodes of disease months after initial discharge, ultimately complicated by fatal meningoencephalitis associated with viral persistence.
Methods
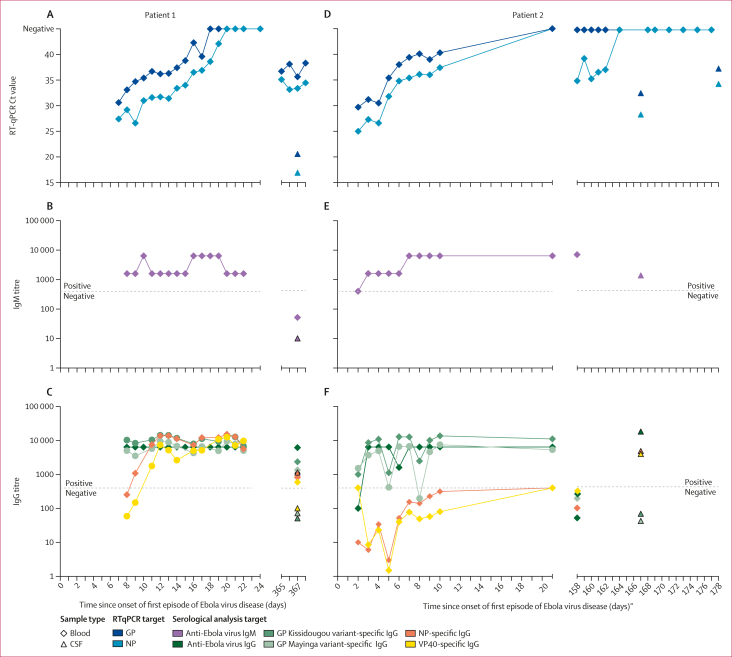
In this case report study, we describe the presentation, management, and subsequent investigations of two patients who developed recrudescent Ebola virus disease and subsequent fatal meningoencephalitis. We obtained data from epidemiological databases, Ebola treatment units, survivor programme databases, laboratory datasets, and hospital records. Following national protocols established during the 2018–20 outbreak in the Democratic Republic of the Congo, blood, plasma, and cerebrospinal fluid (CSF) samples were collected during the first and second episodes of Ebola virus disease from both individuals and were analysed by molecular (quantitative RT-PCR and next-generation sequencing) and serological (IgG and IgM ELISA and Luminex assays) techniques.
Findings
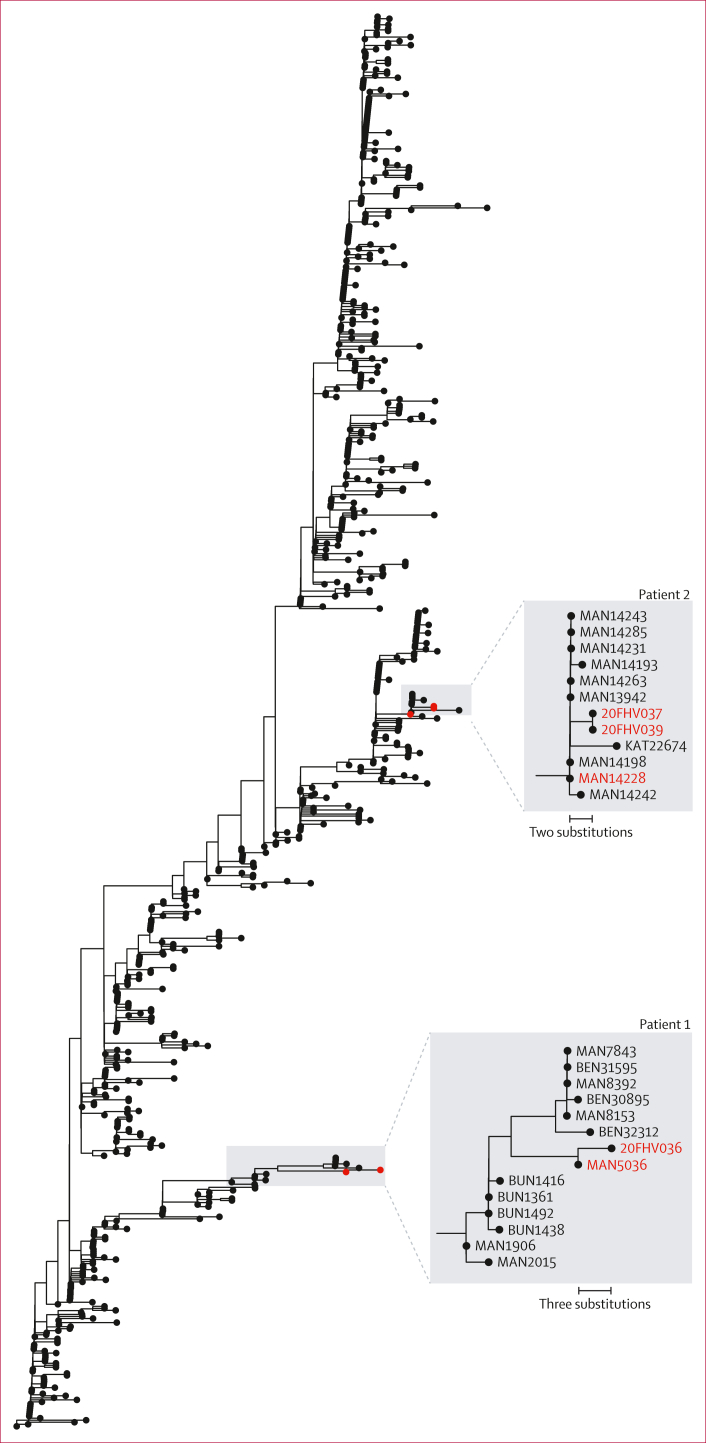
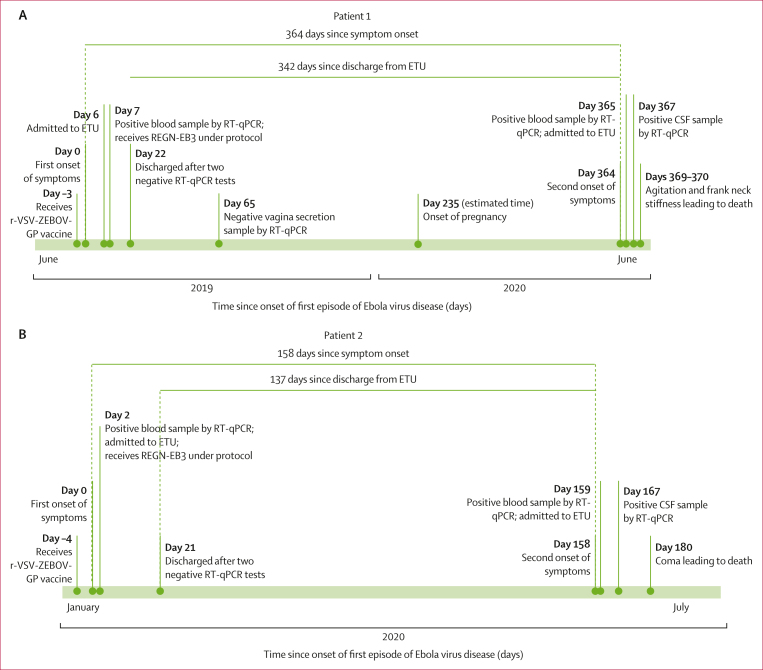
The total time between the end of the first Ebola virus episode and the onset of the second episode was 342 days for patient 1 and 137 days for patient 2. In both patients, Ebola virus RNA was detected in blood and CSF samples during the second episode of disease. Complete genomes from CSF samples from this relapse episode showed phylogenetic relatedness to the genome sequenced from blood samples collected from the initial infection, confirming in-host persistence of Ebola virus. Serological analysis showed an antigen-specific humoral response with typical IgM and IgG kinetics in patient 1, but an absence of an endogenous adaptive immune response in patient 2.
Interpretation
We report the first two cases of fatal meningoencephalitis associated with Ebola virus persistence in two survivors of Ebola virus disease who had received vaccination and mAb-based treatment in the Democratic Republic of the Congo. Our findings highlight the importance of long-term monitoring of survivors, including continued clinical, virological, and immunological profiling, as well as the urgent need for novel therapeutic strategies to prevent and mitigate the individual and public health consequences of Ebola virus persistence.
Funding
Ministry of Health of the Democratic Republic of the Congo, Institut National de Recherche Biomédicale, Infectious Disease Rapid Response Reserve Fund, US Centers for Disease Control and Prevention, US National Cancer Institute (National Institutes of Health), French National Research Institute for Development, and WHO.
刚果民主共和国两名埃博拉病毒病幸存者的致命脑膜脑炎与埃博拉病毒持续存在有关:病例报告研究。
背景:在 2018-20 年刚果民主共和国爆发埃博拉病毒病期间,数以千计的患者接受了前所未有的疫苗接种、单克隆抗体(mAb)治疗或两者兼用,从而产生了大量幸存者。我们旨在报告两名曾接种疫苗并接受过 mAb 治疗的刚果民主共和国埃博拉病毒病幸存者的临床、病毒学、病毒基因组学和免疫学特征:在本病例报告研究中,我们描述了两名埃博拉病毒复发患者的表现、管理和后续调查情况,这两名患者随后患上了致命的脑膜脑炎。我们从流行病学数据库、埃博拉治疗单位、幸存者计划数据库、实验室数据集和医院记录中获取数据。根据 2018-20 年刚果民主共和国疫情爆发期间制定的国家协议,在埃博拉病毒病第一次和第二次发作期间收集了两人的血液、血浆和脑脊液样本,并通过分子(定量 RT-PCR 和下一代测序)和血清学(IgG 和 IgM ELISA 和 Luminex 检测)技术进行了分析:从第一次埃博拉病毒发作结束到第二次发作开始的总时间,1 号患者为 342 天,2 号患者为 137 天。在第二次发病期间,两名患者的血液和脑脊液样本中都检测到了埃博拉病毒 RNA。从这次复发的脑脊液样本中提取的完整基因组与从初次感染时采集的血液样本中测序的基因组显示出系统发育相关性,证实了埃博拉病毒在宿主体内的持续存在。血清学分析显示,患者1出现了抗原特异性体液反应,具有典型的IgM和IgG动力学,但患者2缺乏内源性适应性免疫反应:我们报告了首两例与埃博拉病毒持续存在相关的致命脑膜脑炎病例,这两例病例是在刚果民主共和国接受过疫苗接种和基于 mAb 治疗的埃博拉病毒病幸存者。我们的研究结果突显了对幸存者进行长期监测的重要性,包括持续的临床、病毒学和免疫学分析,以及迫切需要新型治疗策略来预防和减轻埃博拉病毒持续存在对个人和公共卫生造成的后果:资金来源:刚果民主共和国卫生部、国家生物医学研究所、传染病快速反应储备基金、美国疾病控制和预防中心、法国国家发展研究院和世界卫生组织。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Lancet Microbe
Multiple-
CiteScore
27.20
自引率
0.80%
发文量
278
审稿时长
6 weeks
期刊介绍:
The Lancet Microbe is a gold open access journal committed to publishing content relevant to clinical microbiologists worldwide, with a focus on studies that advance clinical understanding, challenge the status quo, and advocate change in health policy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


