Evaluation of HIV antiretroviral treatment adherence in 2019 using anonymized data from the French national health insurance claims data base: The COCOVIH study
Abstract
Objective
Adherence to antiretroviral treatment (ART) plays a key role in achieving viral suppression in people living with HIV. We aimed to quantify ART adherence in the entire French HIV-infected population treated in 2019 and to determine factors of influence.
Methods
People living with HIV were identified using HIV diagnosis according to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision criteria, HIV-specific laboratory tests, and prescription of antiretrovirals in 2019. Adherence was measured using the medication possession ratio (MPR; actual divided by theoretical number of tablets). Variables of interest included sex, age, type of ART, relevant comorbidities, and receiving supplementary universal health coverage for low-income citizens (CMUc).
Results
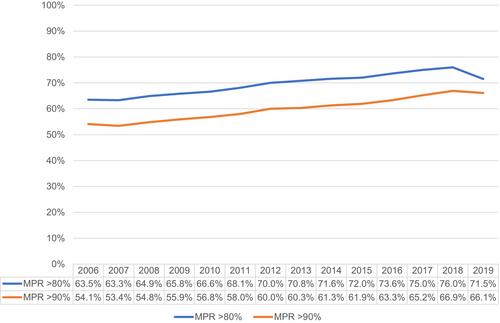
Of the n = 211 124 people living with HIV identified between 2006 and 2019, we included n = 140 607 on ART with two or more prescription fills in 2019 in this analysis. In total, 87.5% of people living with HIV were receiving ART in 2019. Mean ± standard deviation MPR was 82.5 ± 22.7%; 57% of people living with HIV had an MPR ≥90%, and 12.7% had an MPR <50%. Those with an MPR ≥90% significantly differed between males and females (59.1% and 52.8%, respectively; p < 0.001), and between CMUc recipients and non recipients (54.1% and 57.6%, respectively; p < 0.001). MPR ≥90% rate was lower for those with chronic nephropathy (50.2%), renal failure (46.6%), and tuberculosis (50.1%), and for those using psychoactive substances (52.3%). Factors associated with MPR ≥90% in multivariable analysis were older age, male sex, not receiving CMUc, more recent HIV diagnosis, and triple (vs. dual) ART.
Conclusion
In 2019, the average MPR in people living with HIV was 82.5% according to the comprehensive French health care database. Besides sociodemographic variables such as older age, male sex, and not being a CMUc recipient (i.e. of low socioeconomic status), more recent HIV diagnosis and triple therapy were independently associated with better adherence, possibly reflecting advances in ART tolerability and dosing.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


