Impact of Immediate Versus Staged Complete Revascularization on Short-Term and Long-Term Clinical Outcomes in Patients With Acute Coronary Syndrome and Multivessel Disease: A Systematic Review and Meta-Analysis
Abstract
Background
In patients with acute coronary syndrome (ACS) and multivessel disease (MVD), complete revascularization (CR) improves prognosis. This meta-analysis, summarizing recent RCTs, contrasts short-term and long-term clinical outcomes between immediate complete revascularization (ICR) and staged complete revascularization (SCR).
Methods
We systematically searched the online database and eight RCTs were involved. The primary outcomes included long-term unplanned ischemia-driven revascularization, re-infarction, combined cardiovascular (CV) death or myocardial infarction (MI), all-cause death, CV death, stroke, and hospitalization for heart failure (HHF). The secondary outcomes were 1-month unplanned ischemia-driven revascularization, re-infarction, all-cause death, and CV death. Safety endpoints included stent thrombosis and major bleeding.
Results
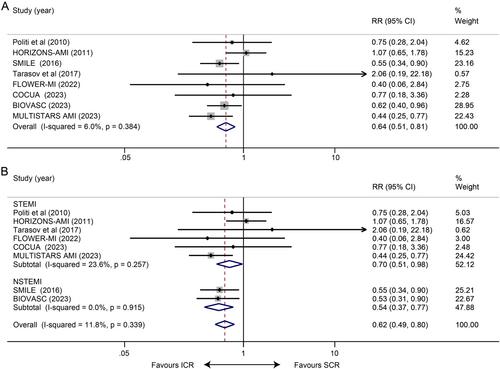
Eight RCTs comprising 5198 patients were involved. ICR reduced long-term unplanned ischemia-driven revascularization (RR 0.64, 95% CI 0.51–0.81, p < 0.001), combined CV death or MI (HR 0.51, 95% CI 0.34–0.78, p = 0.002), and re-infarction (RR 0.66,95% CI 0.48 to 0.91, p = 0.012) compared with SCR. ICR also decreased 1-month unplanned ischemia-driven revascularization (RR 0.41, 95% CI: 0.21–0.77, p = 0.006) and re-infarction (RR 0.33, 95% CI:0.15–0.74, p = 0.007) but increased 1-month all-cause death (RR 2.22, 95% CI 1.06–4.65, p = 0.034).
Conclusion
In ACS patients with MVD, we first found that ICR significantly lowered the risk of both short-term and long-term unplanned ischemia-driven revascularization and re-infarction, as well as the long-term composite outcome of CV death or MI compared with SCR. However, there may be an increase in 1-month all-cause death in the ICR group.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


