Harnessing IL-2 for immunotherapy against cancer and chronic infection: a historical perspective and emerging trends
IF 9.5
2区 医学
Q1 BIOCHEMISTRY & MOLECULAR BIOLOGY
引用次数: 0
Abstract
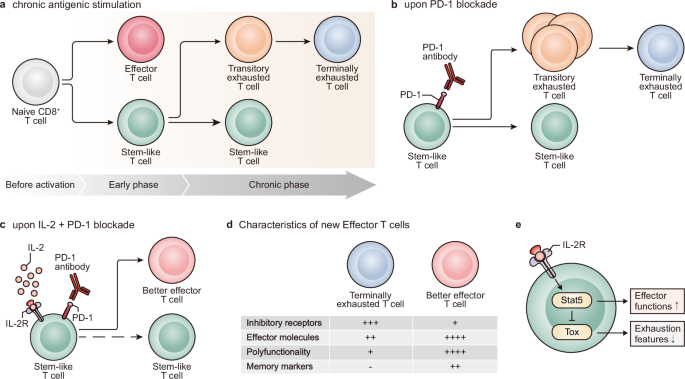
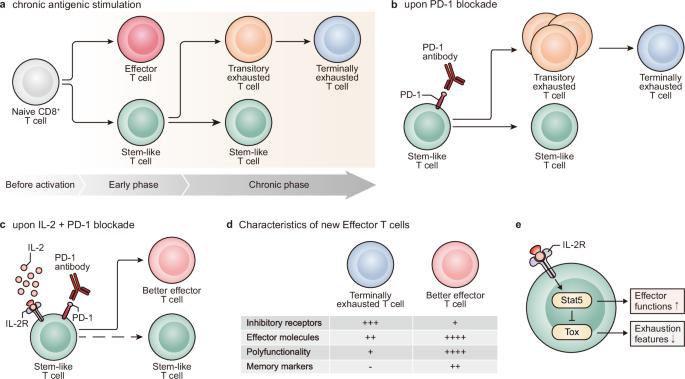
IL-2 therapy, which enhances the function of CD8 + T cells, was initially employed as the cornerstone of immunotherapy against cancer. However, the impact of this therapy extends beyond CD8 + T cells to cells expressing IL-2R, such as endothelial cells and regulatory T cells (Tregs), resulting in various side effects. Consequently, IL-2 therapy has taken a step back from the forefront of treatment. Immune checkpoint inhibitors (ICIs), such as anti-PD-1/PD-L1 antibodies and CTLA-4 antibodies, are used because of their durable therapeutic responses and the reduced incidence of side effects. Nevertheless, only a small fraction of cancer patients respond to ICIs, and research on IL-2 as a combination treatment to improve the efficacy of these ICIs is ongoing. To mitigate side effects, efforts have focused on developing IL-2 variants that do not strongly bind to cells expressing IL-2Rα and favor signaling through IL-2Rβγ. However, recent studies have suggested that, in the context of persistent antigen stimulation models, effective stimulation of antigen-specific exhausted CD8 + T cells in combination with PD-1 inhibitors requires either 1) binding to IL-2Rα or 2) delivery via a fusion with PD-1. This review explores the historical context of IL-2 as an immunotherapeutic agent and discusses future directions for its use in cancer immunotherapy. Interleukin-2 is crucial for combating cancer, but its use is restricted due to severe side effects. This article reviews the development of IL-2 therapy and how it affects CD8 T cells—important immune cells that can become dysfunctional or “exhausted.” To reduce the unwanted effects, researchers have been trying to create a safer version of IL-2 that avoids targeting certain immune and body cells that contribute to these side effects. Recent studies, however, indicate that using the original form of IL-2 or specifically targeting exhausted CD8 T cells with a marker called PD-1 could be more effective in fighting tumors. Additionally, combining IL-2 therapy with PD-1 blockade can enhance T cells response to cancer. These findings suggest a promising future for personalized and effective cancer treatments. This summary was initially drafted using artificial intelligence, then revised and fact-checked by the author.
利用 IL-2 进行癌症和慢性感染免疫治疗:历史视角和新趋势。
IL-2 疗法可增强 CD8 + T 细胞的功能,最初被用作抗癌免疫疗法的基石。然而,这种疗法的影响超出了 CD8 + T 细胞,扩大到表达 IL-2R 的细胞,如内皮细胞和调节性 T 细胞(Tregs),从而导致各种副作用。因此,IL-2疗法从治疗的前沿退了一步。免疫检查点抑制剂(ICIs),如抗PD-1/PD-L1抗体和CTLA-4抗体,因其治疗反应持久、副作用少而被广泛使用。然而,只有一小部分癌症患者对 ICIs 有反应,目前正在研究将 IL-2 作为一种联合疗法,以提高这些 ICIs 的疗效。为了减轻副作用,人们致力于开发 IL-2 的变体,这些变体不会与表达 IL-2Rα 的细胞强烈结合,而是通过 IL-2Rβγ 发出信号。然而,最近的研究表明,在持续性抗原刺激模型中,结合 PD-1 抑制剂有效刺激抗原特异性衰竭的 CD8 + T 细胞需要 1)与 IL-2Rα 结合或 2)通过与 PD-1 融合传递。本综述探讨了 IL-2 作为免疫治疗药物的历史背景,并讨论了其在癌症免疫疗法中的未来应用方向。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Experimental and Molecular Medicine
医学-生化与分子生物学
CiteScore
19.50
自引率
0.80%
发文量
166
审稿时长
3 months
期刊介绍:
Experimental & Molecular Medicine (EMM) stands as Korea's pioneering biochemistry journal, established in 1964 and rejuvenated in 1996 as an Open Access, fully peer-reviewed international journal. Dedicated to advancing translational research and showcasing recent breakthroughs in the biomedical realm, EMM invites submissions encompassing genetic, molecular, and cellular studies of human physiology and diseases. Emphasizing the correlation between experimental and translational research and enhanced clinical benefits, the journal actively encourages contributions employing specific molecular tools. Welcoming studies that bridge basic discoveries with clinical relevance, alongside articles demonstrating clear in vivo significance and novelty, Experimental & Molecular Medicine proudly serves as an open-access, online-only repository of cutting-edge medical research.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


