Treatment engagement in comorbid alcohol use disorder and alcohol-related liver disease: A qualitative exploration of barriers and facilitators with service users
Abstract
Background
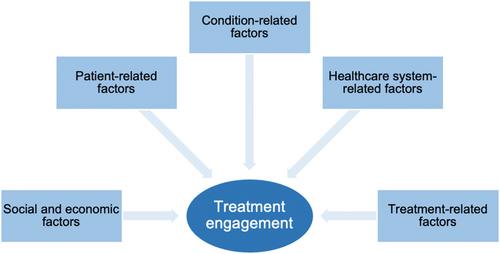
Effective interventions to improve patient outcomes in comorbid alcohol use disorder (AUD) and alcohol-related liver disease (ARLD) remain a clinical unmet need. While the choice of abstinence is the cornerstone for the prevention of disease progression and mortality, evidence suggests a suboptimal engagement with treatment supporting recovery. This qualitative investigation aims to understand barriers and facilitators to treatment as experienced by this clinical population by applying a multidimensional adherence model proposed by the World Health Organization.
Methods
Twenty-four participants with comorbid AUD and ARLD were recruited from an inpatient clinical setting. Data for this study were collected through semistructured, in-depth interviews. Deductive analysis was organized by the Framework method, and theory-driven themes were identified according to the multidimensional adherence model. This included factors across the social and economic, patient, condition, treatment, and healthcare system levels.
Results
The findings in this study indicate systematic challenges in maintaining continuity between primary, secondary, and community care. Aspects related to social and economic context, treatment, and healthcare systems were found to hinder engagement. Identified facilitators to engagement included the participatory role of family, shared lived experience of addiction/recovery, and therapeutic alliance with healthcare providers.
Conclusion
The understanding of these barriers and facilitators from a service user's perspective can bridge the treatment gap for this clinical population. This can provide an opportunity for the implementation of effective interventions and inform the development of policies promoting accessible care. Government and public health bodies have fundamental roles in shifting treatment paradigms in comorbid AUD and ARLD.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


