Physical Health Checks and Follow-Up Care in Deprived and Ethnically Diverse People With Severe Mental Illness: Co-Designed Recommendations for Better Care
Abstract
Background
There is wide variation in premature mortality rates in adults with severe mental illness (SMI) across London, with Tower Hamlets (a highly deprived and ethnically diverse area) scoring the highest.
Objective
To identify examples of best practice and co-design recommendations for improving physical health checks and follow-up care amongst people with SMI in Tower Hamlets.
Methods
Data were collected through online questionnaires (using SMI physical health best practice checklists), one-on-one interviews (n = 7) and focus groups (n = 3) with general practices, secondary mental health services, commissioners and leads of community services and public health programmes, experts by experience and community, voluntary and social enterprise organisations in Tower Hamlets. Data were analysed using deductive and inductive thematic analysis.
Results
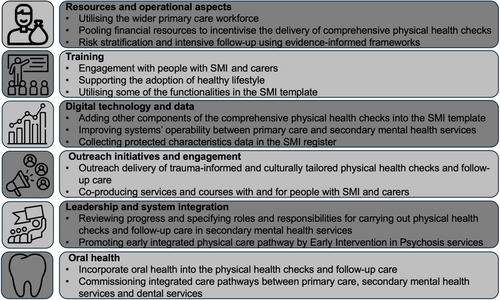
Twenty-two participants representing 15 general practices (out of 32), secondary mental health services, commissioners and public health leads completed the online questionnaires. Twenty-one participants took part in interviews and focus groups. Examples of best practice included cleaning and validating the SMI register regularly by general practices, knowing the number of patients who had been offered and/or received physical health checks, having clear pathways to community and specialist care services, using various communication methods and having a key performance indicator (KPI) for tailored smoking cessation services for people with SMI. Recommendations included adopting evidence-informed frameworks for risk stratification and utilising the wider primary care workforce with specific training to follow up on results, offer interventions and support navigating pathways and taking up follow-up care. Incentivising schemes were needed to deliver additional physical health check components such as oral health, cancer screening, Covid-19 vaccination and sexual health checks. Including KPIs in other community services' specifications with reference to SMI people was warranted. Further engagement with experts by experience and staff training were needed.
Conclusion
The present initiative identified best practice examples and co-designed recommendations for improving physical health checks and follow-up care in deprived and ethnically diverse people with SMI.
Patient or Public Contribution
This initiative was supported by three experts with experience, and two community organisations, who were involved in data curation and interpretation, development of recommendations and/or dissemination activities including writing this manuscript.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


