Likely causal effects of insulin resistance and IGF-1 bioaction on childhood and adult adiposity: a Mendelian randomization study
IF 4.2
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
Abstract
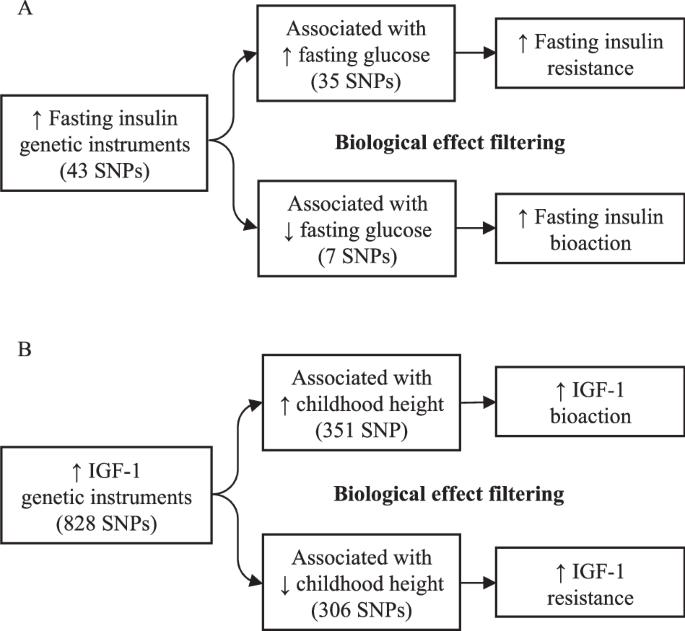
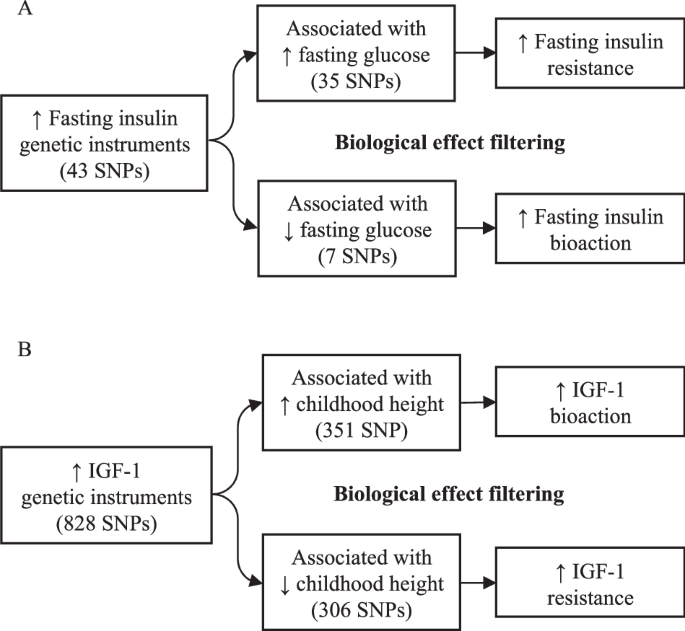
Circulating insulin and insulin-like growth factor-1 (IGF-1) concentrations are positively correlated with adiposity. However, the causal effects of insulin and IGF-1 on adiposity are unclear. We performed two-sample Mendelian randomization analyses to estimate the likely causal effects of fasting insulin and IGF-1 on relative childhood adiposity and adult body mass index (BMI). To improve accuracy and biological interpretation, we applied Steiger filtering (to avoid reverse causality) and ‘biological effect’ filtering of fasting insulin and IGF-1 associated variants. Fasting insulin-increasing alleles (35 variants also associated with higher fasting glucose, indicative of insulin resistance) were associated with lower relative childhood adiposity (P = 3.8 × 10−3) and lower adult BMI (P = 1.4 × 10−5). IGF-1-increasing alleles also associated with taller childhood height (351 variants indicative of greater IGF-1 bioaction) showed no association with relative childhood adiposity (P = 0.077) or adult BMI (P = 0.562). Conversely, IGF-1-increasing alleles also associated with shorter childhood height (306 variants indicative of IGF-1 resistance) were associated with lower relative childhood adiposity (P = 6.7 × 10−3), but effects on adult BMI were inconclusive. Genetic causal modelling indicates negative effects of insulin resistance on childhood and adult adiposity, and negative effects of IGF-1 resistance on childhood adiposity. Our findings demonstrate the need to distinguish between bioaction and resistance when modelling variants associated with biomarker concentrations.
胰岛素抵抗和 IGF-1 生物作用对儿童和成人肥胖的可能因果效应:孟德尔随机研究。
背景:循环中胰岛素和胰岛素样生长因子-1(IGF-1)的浓度与脂肪率呈正相关。然而,胰岛素和 IGF-1 对肥胖的因果效应尚不清楚:我们进行了双样本孟德尔随机分析,以估计空腹胰岛素和 IGF-1 对相对儿童脂肪率和成人体重指数(BMI)的可能因果效应。为了提高准确性和生物学解释,我们对空腹胰岛素和IGF-1相关变异进行了Steiger过滤(以避免反向因果关系)和 "生物效应 "过滤:结果:空腹胰岛素增加等位基因(35 个变异也与空腹血糖升高有关,表明胰岛素抵抗)与较低的儿童相对脂肪率(P = 3.8 × 10-3)和较低的成人体重指数(P = 1.4 × 10-5)有关。同样与儿童身高有关的 IGF-1 增高等位基因(351 个表明 IGF-1 生物作用更强的变体)与儿童相对脂肪率(P = 0.077)或成人体重指数(P = 0.562)没有关联。相反,IGF-1增加的等位基因也与儿童身高较矮有关(306个变异表明IGF-1抗性),但与较低的儿童相对脂肪率有关(P = 6.7 × 10-3),但对成人体重指数的影响尚无定论:遗传因果建模表明,胰岛素抵抗对儿童期和成年期肥胖有负面影响,IGF-1抵抗对儿童期肥胖有负面影响。我们的研究结果表明,在建立与生物标志物浓度相关的变异模型时,需要区分生物作用和抵抗作用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


