Survey on the knowledge and practices in anorexia of aging diagnosis and management in Japan
Abstract
Background
Anorexia of aging (AA) is a condition in older adults that includes loss of appetite and reduced food intake. There is a lack of detailed analysis of the potential influence of educational initiatives in addressing AA. This study aimed to clarify the current state of knowledge and practice regarding AA and its relationship with the availability of continuing education opportunities among Japanese healthcare professionals involved in treating older patients.
Methods
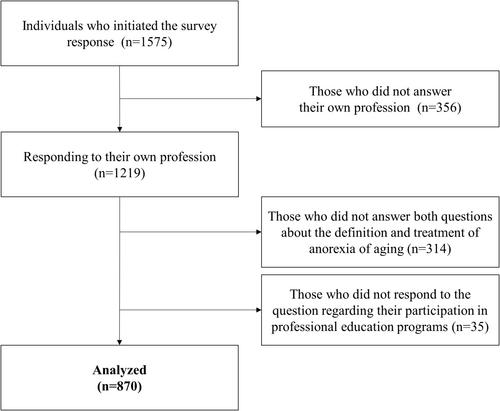
The Japan Geriatrics Society and the Japanese Association on Sarcopenia and Frailty, in collaboration with the Society on Sarcopenia, Cachexia, and Wasting Disorders, conducted an online questionnaire survey on the knowledge and practices in AA detection and management. Questions were asked in the areas of demographics, screening, definition/diagnosis, treatment, referral, and awareness, with those who ‘participate’ in continuing education and professional development programmes in nutrition for their patients were classified as the ‘education group’ and those who ‘do not participate’ were classified as the ‘non-education group’. The results for each question were compared.
Results
The analysis included 870 participants (physicians, 48%; registered dietitians, 16%; rehabilitation therapists, 14%; pharmacists, 12%; nurses, 6%; and other professionals, 5%). The education group (45%) was more likely than the non-education group (55%) to use the Mini-Nutritional Assessment Short Form (MNA-SF) to screen for AA (49% vs. 27%) and less likely not to use a validated tool (33% vs. 47%). More participants used evidence-based tools and materials for AA care (38% vs. 12%), and fewer used their clinical judgement (23% vs. 35%) or were unaware of the tools and materials (9% vs. 23%). The proportion using a team of professionals experienced in AA care were 47% and 24% of the education and non-education groups, respectively. By profession, few physicians used specific validated tools and resources for AA screening and treatment. More than half of the dietitians used the MNA-SF regardless of training opportunity availability. Regarding professional availability and team use, differences in educational opportunities were particularly large among physicians.
Conclusions
Participation in continuing education programmes on nutrition is associated with responsiveness to AA screening and treatment and the availability of a team of professionals, which may influence the quality of AA treatment. Nutrition education may support the confidence of healthcare professionals working with older adults in AA with complex clinical signs and encourage them to conduct evidence-based practice.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


