Polygenic score for body mass index in relation to mortality among patients with renal cell cancer
IF 4.2
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
Abstract
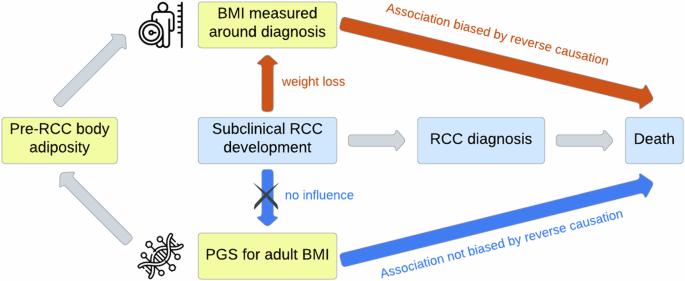
The association between body mass index (BMI) and mortality among individuals with renal cell cancer (RCC) is debated, with some observational studies suggesting a lower mortality associated with higher BMI. However, methodological issues such as confounding and reverse causation may bias these findings. Using BMI-associated genetic variants can avoid these biases and generate more valid estimates. In this prospective cohort study, we included 1264 RCC patients (446 deaths) from the UK Biobank. We created a BMI polygenic score (PGS) based on 336 BMI-associated genetic variants. The association between the PGS and mortality (all-cause and RCC-specific) was evaluated by logistic regression (all RCC cases) and Cox regression (906 incident cases). For comparison, the associations of measured pre-diagnostic BMI and waist-to-hip ratio (WHR) with mortality were quantified by Cox regression among incident cases. We stratified these analyses by time between anthropometric measurement and RCC diagnosis to assess the influence of reverse causation. We did not observe an association between the BMI PGS and all-cause mortality among RCC patients (hazard ratio (HR) per SD increase = 0.98, 95% CI: 0.88,1.10). No association was found for pre-diagnostic BMI (HR per 5 kg/m2 increase = 0.93, 95% CI: 0.83,1.04) or WHR (HR per 0.1 increase = 0.97, 95% CI: 0.83,1.13) with mortality. In patients with anthropometrics measured within 2 years before RCC diagnosis, we observed associations of higher BMI (HR per 5 kg/m2 = 0.76, 95% CI: 0.59,0.98) and WHR (HR = 0.67 per 0.1 increase, 95% CI: 0.45,0.98) with a lower risk of death. Similar patterns were observed for RCC-specific mortality. We found no association between either genetic variants for high BMI or measured pre-diagnostic body adiposity and mortality among RCC patients, and our results suggested a role for reverse causation in the association of obesity with lower mortality. Future studies should be designed carefully to produce unbiased estimates that account for confounding and reverse causation.

肾细胞癌患者体重指数的多基因评分与死亡率的关系。
背景:体重指数(BMI)与肾细胞癌(RCC)患者死亡率之间的关系存在争议,一些观察性研究表明,体重指数越高,死亡率越低。然而,混杂和反向因果关系等方法学问题可能会使这些研究结果产生偏差。使用与 BMI 相关的基因变异可避免这些偏差,并得出更有效的估计结果:在这项前瞻性队列研究中,我们纳入了英国生物库中的 1264 例 RCC 患者(死亡 446 例)。我们根据 336 个与 BMI 相关的遗传变异创建了 BMI 多基因评分(PGS)。我们通过逻辑回归(所有 RCC 病例)和 Cox 回归(906 例发病病例)评估了 PGS 与死亡率(全因死亡率和 RCC 特异性死亡率)之间的关系。为了进行比较,我们通过 Cox 回归量化了诊断前体重指数(BMI)和腰臀比(WHR)与病例死亡率之间的关系。我们按照人体测量与 RCC 诊断之间的时间间隔对这些分析进行了分层,以评估反向因果关系的影响:结果:我们没有观察到 BMI PGS 与 RCC 患者的全因死亡率之间存在关联(每增加 SD 的危险比 (HR) = 0.98,95% CI:0.88,1.10)。诊断前 BMI(每增加 5 kg/m2 的 HR = 0.93,95% CI:0.83,1.04)或 WHR(每增加 0.1 的 HR = 0.97,95% CI:0.83,1.13)与死亡率没有关联。在 RCC 诊断前 2 年内测量过人体测量指标的患者中,我们观察到较高的 BMI(每增加 5 kg/m2 的 HR = 0.76,95% CI:0.59,0.98)和 WHR(每增加 0.1 的 HR = 0.67,95% CI:0.45,0.98)与较低的死亡风险相关。RCC特异性死亡率也观察到类似的模式:我们没有发现高体重指数的遗传变异或诊断前身体脂肪含量的测量值与 RCC 患者的死亡率之间存在关联,我们的研究结果表明,肥胖与降低死亡率之间存在反向因果关系。今后的研究应精心设计,以得出考虑到混杂因素和反向因果关系的无偏估计值。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


