Intestinal microbiology and urinary tract infection associated risk in long-term aged care residents
IF 5.4
Q1 MEDICINE, RESEARCH & EXPERIMENTAL
引用次数: 0
Abstract
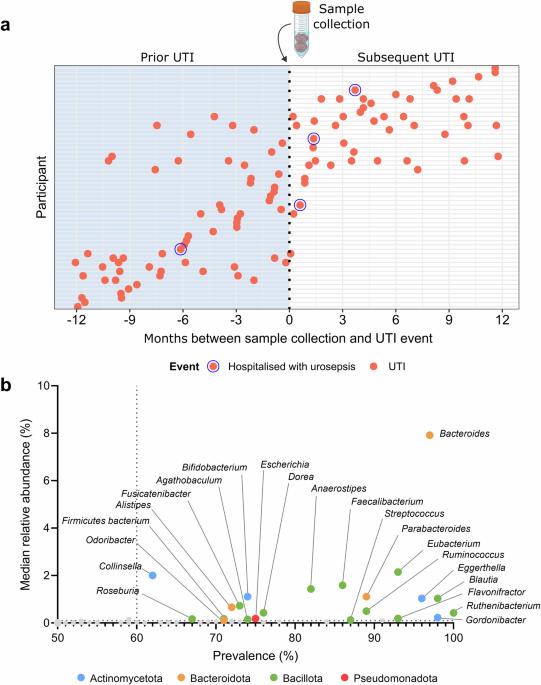
Urinary tract infections (UTI) are the most frequently diagnosed infection in residents of long-term care and are a major risk factor for urosepsis, hospitalisation, and death. Translocation of gut pathobionts into the urinary tract is the presumed cause of most UTIs. While specific gut microbiota characteristics have been linked to UTI risk in younger adults, their relevance in aged care residents remains uncertain. The faecal microbiome was assessed in 54 long-term aged care residents with a history of UTIs and 69 residents without a UTI history. Further comparisons were made to microbiome characteristics in 20 younger adults without UTIs. Microbiome characteristics were examined in relation to prior and subsequent UTIs, as well as antibiotic therapy. In long-term aged care residents, prior UTI history and exposure to UTI-exclusive antibiotics do not significantly affect microbiome composition or functional capacity. However, exposure to antibiotics unrelated to UTI treatment is associated with distinct microbiota compositional traits. Adjustment for dementia, incontinence, diabetes, and prior antibiotic use finds no microbiota characteristic linked to UTI development. However, prior UTI is identified as a predictor of future UTIs. Comparison with younger adults identifies greater within-participant dispersion in aged care residents, as well as lower microbiota diversity and altered microbiome functional potential. No association between the gut microbiome and UTI incidence, as has been reported in younger individuals, is evident in long-term aged care residents. Considerable variability in gut microbiome characteristics, relating to high antibiotic exposure and age-related physiological and immunological factors, could mask such a relationship. However, it cannot be discounted that increased UTI risk in the elderly is independent of microbiome-mediated mechanisms. Urinary tract infections (UTIs) are common in residents of long-term aged care facilities, posing serious health risks. Harmful bacteria moving from the gut to the urinary tract is thought to cause most UTIs. It is still unclear, however, how differences in gut bacteria contribute to UTI risk in older adults. Here, we investigate the gut bacteria of aged care residents, both with and without a history of UTIs, and compare them to younger adults. While prior UTIs did not alter gut bacteria, antibiotic use did. We observed greater variability in gut bacteria among aged care residents compared to younger adults. These observations suggest that both high antibiotic exposure and age-related factors may mask any potential relationship between gut bacteria and UTI risk in this population. Understanding these factors could lead to improved UTI prevention and treatment strategies for elderly individuals. Miller et al. investigate the gut microbiome in long-term aged care residents with and without UTI history, as well as younger adults. Findings reveal considerable variability in gut microbiome characteristics due to age-related factors which may mask microbiome-UTI associations.
长期老年护理居民的肠道微生物与尿路感染相关风险
尿路感染(UTI)是长期护理住院患者中最常见的感染,也是导致尿毒症、住院和死亡的主要风险因素。肠道病原菌转移到泌尿道是大多数尿路感染的假定原因。虽然特定的肠道微生物群特征与年轻人患尿毒症的风险有关,但它们与老年护理居民的相关性仍不确定。我们对 54 位有尿毒症病史的长期老年护理居民和 69 位无尿毒症病史的居民的粪便微生物群进行了评估。此外,还对 20 名未患尿毒症的年轻人的微生物组特征进行了比较。微生物组特征与之前和之后的 UTI 以及抗生素治疗有关。在长期老年护理居民中,既往尿毒症病史和接触过尿毒症专用抗生素不会对微生物组的组成或功能能力产生重大影响。然而,接触与UTI治疗无关的抗生素与不同的微生物群组成特征有关。在对痴呆症、尿失禁、糖尿病和以前使用抗生素的情况进行调整后,没有发现微生物群特征与UTI的发展有关。不过,以前患过尿毒症被认为是未来患尿毒症的一个预测因素。与年轻人相比,老年护理居民的微生物群内部分散性更大,微生物群多样性更低,微生物群的功能潜力也有所改变。在长期老年护理居民中,肠道微生物组与UTI发病率之间没有明显的联系,这一点在年轻人中已有报道。肠道微生物组特征的巨大变异与大量抗生素接触以及与年龄相关的生理和免疫因素有关,可能会掩盖这种关系。但是,不能排除老年人UTI风险增加与微生物组介导的机制无关。尿路感染(UTI)在长期老年护理机构的居民中很常见,对健康构成严重威胁。有害细菌从肠道转移到泌尿道被认为是导致大多数尿路感染的原因。然而,目前还不清楚肠道细菌的差异是如何导致老年人UTI风险的。在这里,我们调查了有过和没有过尿毒症病史的老年护理居民的肠道细菌,并将其与年轻人进行了比较。虽然既往尿毒症病史不会改变肠道细菌,但使用抗生素却会。与年轻人相比,我们观察到老年护理住院患者肠道细菌的变化更大。这些观察结果表明,高抗生素暴露率和与年龄相关的因素可能会掩盖这一人群中肠道细菌与 UTI 风险之间的任何潜在关系。了解这些因素可以改进老年人的 UTI 预防和治疗策略。米勒等人调查了有UTI病史和无UTI病史的长期老年护理居民以及年轻成年人的肠道微生物组。研究结果显示,由于年龄相关因素,肠道微生物组的特征存在相当大的变异性,这可能会掩盖微生物组与UTI之间的关联。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


