Intraocular pressure, primary open-angle glaucoma and the risk of retinal vein occlusion: A Mendelian randomization mediation analysis
IF 2.8
3区 医学
Q1 OPHTHALMOLOGY
引用次数: 0
Abstract
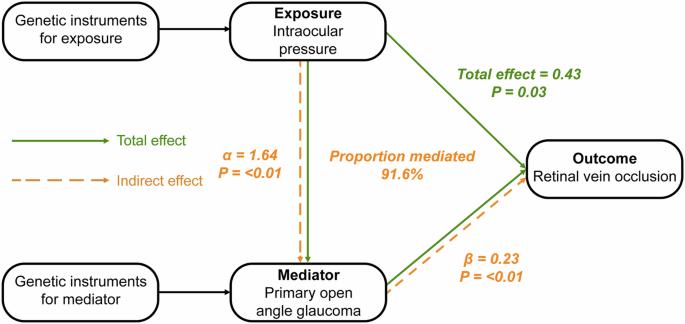
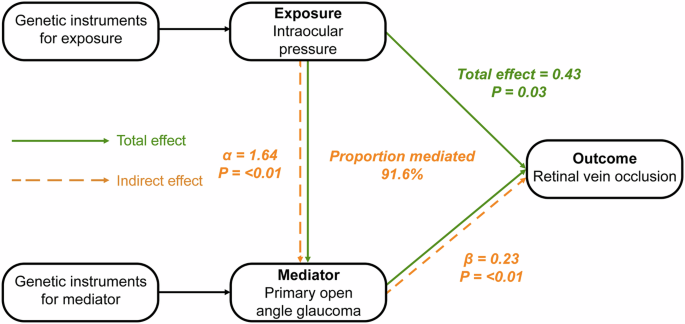
The etiological connection between intraocular pressure (IOP) and the risk of retinal vein occlusion (RVO) remains elusive, particularly regarding whether this risk emanates from the direct influence of elevated intraocular pressure (IOP), irrespective of the presence of primary open-angle glaucoma (POAG), or if it arises as a consequence of the sequelae of POAG. Therefore, we conducted a Mendelian Randomization (MR) mediation analysis to elucidate the mediating role of POAG in the association between IOP and RVO. We identified 47 single-nucleotide polymorphisms (SNPs) associated with IOP (P-value < 5 × 10−8) leveraging data from a genome-wide association study (GWAS) (N = 97,653) obtained from the UK Biobank and 50 SNPs associated with POAG (P-value < 5 × 10−8) from a GWAS meta-analysis (16,677 cases and 199,580 controls). We related these SNPs with RVO using a GWAS of 775 RVO cases and 376,502 controls from FinnGen. By utilizing univariable and multivariable MR analyses we calculated the total effect of IOP on RVO and estimated the degree to which POAG mediates this association. MR analyses showed that higher IOP is associated with higher RVO risk (odds ratio of RVO per 1 mmHg increase in IOP: 1.53; 95% confidence interval: 1.04 to 2.26; p-value = 0.03). Moreover, our MR mediation analysis suggested that 91.6% of the total effect of IOP on RVO risk was mediated through POAG. The primary results were consistent with estimates of pleiotropy-robust MR methods. Our findings suggest that higher IOP increases the risk of RVO and that the majority of this effect is mediated through POAG.
眼压、原发性开角型青光眼和视网膜静脉闭塞的风险:孟德尔随机化中介分析。
背景:眼压(IOP)与视网膜静脉闭塞(RVO)风险之间的病因学联系仍然难以捉摸,特别是关于这种风险是来自眼压(IOP)升高的直接影响(无论是否存在原发性开角型青光眼(POAG)),还是作为 POAG 后遗症的结果。因此,我们进行了孟德尔随机化(Mendelian Randomization,MR)中介分析,以阐明 POAG 在 IOP 与 RVO 关联中的中介作用:我们利用从英国生物库(UK Biobank)获得的全基因组关联研究(GWAS)数据(N = 97,653),确定了与眼压相关的 47 个单核苷酸多态性(SNPs)(P 值 -8),并从 GWAS 元分析(16,677 例病例和 199,580 例对照)中确定了与 POAG 相关的 50 个 SNPs(P 值 -8)。通过单变量和多变量 MR 分析,我们计算了眼压对 RVO 的总影响,并估计了 POAG 在多大程度上介导了这种关联:磁共振分析表明,眼压越高,RVO 风险越高(眼压每升高 1 mmHg,RVO 的几率比:1.53;95% 置信区间:1.04 至 2.26;P 值 = 0.03)。此外,我们的 MR 中介分析表明,在 IOP 对 RVO 风险的总影响中,91.6% 是通过 POAG 中介的。主要结果与多向性稳健磁共振方法的估计结果一致:我们的研究结果表明,较高的眼压会增加罹患 RVO 的风险,而这种影响的大部分是通过 POAG 介导的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Eye
医学-眼科学
CiteScore
6.40
自引率
5.10%
发文量
481
审稿时长
3-6 weeks
期刊介绍:
Eye seeks to provide the international practising ophthalmologist with high quality articles, of academic rigour, on the latest global clinical and laboratory based research. Its core aim is to advance the science and practice of ophthalmology with the latest clinical- and scientific-based research. Whilst principally aimed at the practising clinician, the journal contains material of interest to a wider readership including optometrists, orthoptists, other health care professionals and research workers in all aspects of the field of visual science worldwide. Eye is the official journal of The Royal College of Ophthalmologists.
Eye encourages the submission of original articles covering all aspects of ophthalmology including: external eye disease; oculo-plastic surgery; orbital and lacrimal disease; ocular surface and corneal disorders; paediatric ophthalmology and strabismus; glaucoma; medical and surgical retina; neuro-ophthalmology; cataract and refractive surgery; ocular oncology; ophthalmic pathology; ophthalmic genetics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


