Olfactory perceptual fingerprints of people with olfactory dysfunction and healthy controls
Abstract
Objective(s)
An olfactory perceptual fingerprint (OPF) defines one's olfactory perception using perceptual descriptor ratings (such as odor pleasantness, intensity) for a set of odors. OPFs have been shown to distinguish patients with COVID-related olfactory dysfunction (OD) and healthy controls with 86% accuracy. However, all participants rated the same odorants. With the aim to evaluate whether the OPFs are indeed odorant independent, previously published dataset by Lötsch et al. was reanalyzed. Furthermore, this independent dataset was used to check whether the OPFs separate patients with OD due to various causes from controls.
Methods
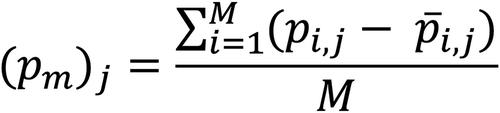
The study included 104 controls and 42 patients, who were randomized into four odor sets with 10 odorants each. Odorants were presented using a computer-controlled olfactometer and evaluated on scales from 1 (not at all) to 5 (very) using perceptual descriptors pleasant, intensive, familiar, edible, irritating, cold/warm, and painful.
Results
Permutational multivariate analysis of variance showed that the odor set did not have a significant effect on the OPFs, confirming that the OPFs are indeed odorant independent. On the other hand, both diagnosis and age affected the OPFs (p < .001) and explained around 11% and 5% of the variance of the OPFs, respectively. Furthermore, a supervised machine learning method, random forest classifier, showed that OPF can distinguish patients and controls with 80% accuracy.
Conclusion
OPFs are odorant independent. Patients perceived odors as less familiar, less intense, and less edible than controls. Other perceptual descriptors were much less important for the separation of patients and controls.
Level of evidence
3

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


