Prevalence and patterns of methamphetamine use and mental health disparity in the United States
引用次数: 0
Abstract
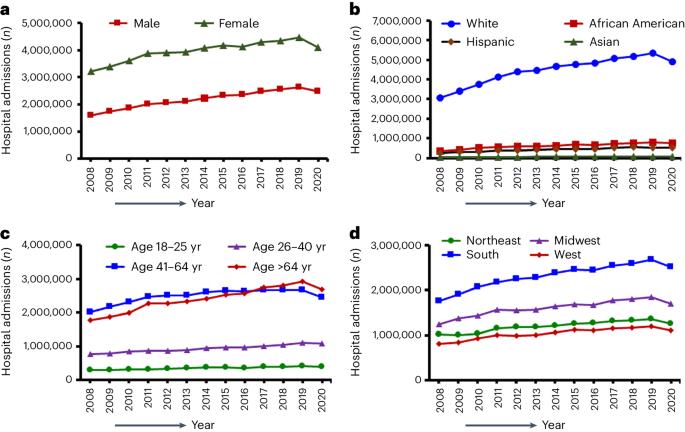
Methamphetamine is a growing health problem, as is mental health illness. However, no studies have investigated the combinatory effects of both diseases or characterized national trends over a period of time greater than 10 years. We evaluated US trends in mental health disorder-related hospital admissions (MHD-HAs) and compared them with those with concurrent methamphetamine use (MHD-HA-MUs), comparing the demographic characteristics from 2008 to 2020. Our findings reveal a significant increase in MHD-HA-MUs, increasing 10.5-fold, compared with a 1.4-fold increase in MHD-HAs. We also found a 1.53 times higher adjusted prevalence ratio of MHD-HA-MUs compared with MHD-HAs, even when adjusted for confounding factors. MHD-HA-MUs increased significantly among male patients (13-fold), non-Hispanic Black patients (39-fold), those aged 41–64 years (16-fold), and the South (24-fold). Overall, the data suggest that there are synergistic effects with methamphetamine use and mental health disorder, highlighting this patient group’s unique needs, requiring distinct action. Investigating the influence of using methamphetamine on the rate of admissions for mental health disorders, this study finds that concurrent methamphetamine use increased mental health-related hospital admissions 10.5-fold. Increased prevalence was also found for men, non-Hispanic Black people, middle-aged adults, and people living in the South.
美国使用甲基苯丙胺的流行率和模式以及心理健康差异
与精神疾病一样,甲基苯丙胺也是一个日益严重的健康问题。然而,还没有研究调查过这两种疾病的综合影响,也没有研究描述过 10 年以上的全国趋势。我们评估了美国与精神疾病有关的入院人数(MHD-HA)趋势,并将其与同时吸食甲基苯丙胺的入院人数(MHD-HA-MUs)进行了比较,同时比较了 2008 年至 2020 年的人口特征。我们的研究结果显示,MHD-HA-MUs 大幅增加,增加了 10.5 倍,而 MHD-HAs 只增加了 1.4 倍。我们还发现,经调整后,MHD-HA-MU 的患病率比 MHD-HA 高出 1.53 倍,即使对混杂因素进行调整也是如此。男性患者(13 倍)、非西班牙裔黑人患者(39 倍)、41-64 岁人群(16 倍)和南方人(24 倍)中的 MHD-HA-MUs 显著增加。总体而言,这些数据表明,吸食甲基苯丙胺和精神疾病会产生协同效应,凸显了这一患者群体的独特需求,需要采取不同的行动。本研究调查了吸食甲基苯丙胺对精神疾病入院率的影响,发现同时吸食甲基苯丙胺会使精神疾病相关入院率增加 10.5 倍。研究还发现,男性、非西班牙裔黑人、中年人和居住在南方的人的发病率也有所上升。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


