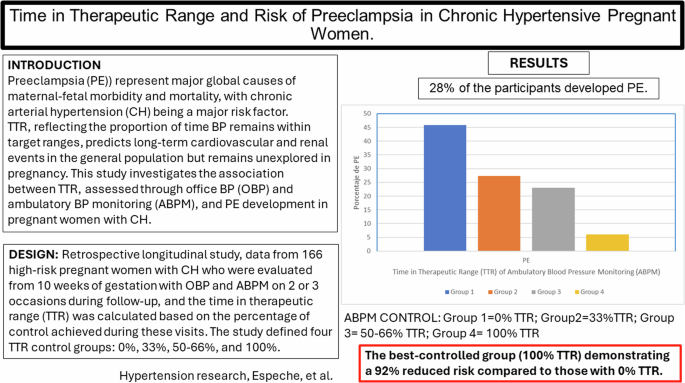
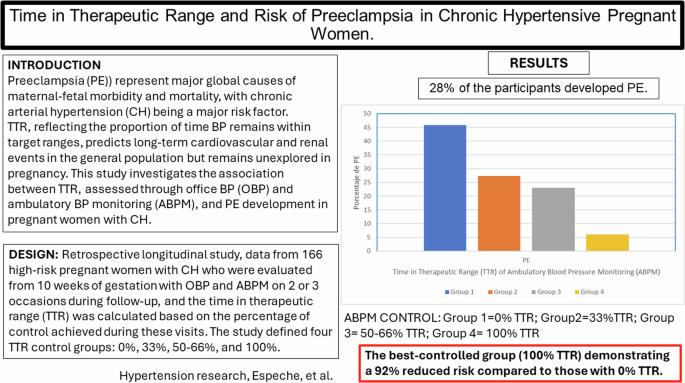
Time in therapeutic range and risk of preeclampsia in chronic hypertensive pregnant women
IF 4.3
2区 医学
Q1 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
Pregnancy Hypertensive Disorders (PHD), particularly Preeclampsia (PE), are significant contributors to maternal-fetal morbidity and mortality, with chronic arterial hypertension (CH) being a major risk factor. The prevalence of CH has risen alongside obesity and advanced maternal age. While antihypertensive treatment mitigates adverse pregnancy outcomes, the duration of effective blood pressure (BP) control, termed Time in Therapeutic Range (TTR), has not been extensively studied in pregnant women. TTR, reflecting the proportion of time BP remains within target ranges, predicts long-term cardiovascular and renal events in the general population but remains unexplored in pregnancy. This study investigates the association between TTR, assessed through office BP (OBP) and ambulatory BP monitoring (ABPM), and PE development in pregnant women with CH. In a retrospective longitudinal study, data from 166 pregnant women with HA referred to our hospital analyzed. BP was measured using OBP and ABPM from 10 weeks of gestation, with TTR calculated as the percentage of visits where BP remained within target ranges. The study defined four TTR control groups: 0%, 33%, 50–66%, and 100%. Results showed that 28% of the participants developed PE, with a higher incidence correlating with lower TTR in ABPM. TTR in ABPM was a significant predictor of PE risk, with the best-controlled group (100% TTR) demonstrating a 92% reduced risk compared to those with 0% TTR. The agreement between OBP and ABPM TTR was low, emphasizing the importance of ABPM for accurate BP monitoring in pregnancy. This study indicates that integrating ABPM for TTR assessment in high-risk pregnancies has the potential to reduce maternal and fetal complications.
慢性高血压孕妇在治疗范围内的时间与先兆子痫的风险。
妊娠期高血压疾病(PHD),尤其是子痫前期(PE),是导致母胎发病率和死亡率的重要因素,其中慢性动脉高血压(CH)是一个主要风险因素。随着肥胖和高龄产妇的增加,慢性动脉高血压的发病率也在上升。虽然降压治疗可减轻不良妊娠结局,但有效控制血压(BP)的持续时间,即治疗范围内时间(TTR),尚未在孕妇中进行广泛研究。TTR 反映了血压保持在目标范围内的时间比例,可预测普通人群的长期心血管和肾脏事件,但在妊娠期仍未进行研究。本研究调查了通过诊室血压(OBP)和非卧床血压监测(ABPM)评估的 TTR 与患有心脏病的孕妇发生 PE 之间的关系。在一项回顾性纵向研究中,我们分析了转诊至本院的166名妊娠合并HA的孕妇的数据。从妊娠 10 周开始使用 OBP 和 ABPM 测量血压,并根据血压保持在目标范围内的就诊百分比计算 TTR。研究定义了四个 TTR 对照组:0%、33%、50-66% 和 100%。结果显示,28% 的参与者发生了 PE,发病率较高与 ABPM 的 TTR 较低有关。ABPM 中的 TTR 是预测 PE 风险的一个重要指标,与那些 TTR 为 0% 的人相比,最佳控制组(TTR 为 100%)的风险降低了 92%。OBP 和 ABPM TTR 之间的一致性很低,这强调了 ABPM 对准确监测妊娠期血压的重要性。这项研究表明,在高危妊娠中结合 ABPM 评估 TTR 有可能减少孕产妇和胎儿的并发症。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Hypertension Research
医学-外周血管病
CiteScore
7.40
自引率
16.70%
发文量
249
审稿时长
3-8 weeks
期刊介绍:
Hypertension Research is the official publication of the Japanese Society of Hypertension. The journal publishes papers reporting original clinical and experimental research that contribute to the advancement of knowledge in the field of hypertension and related cardiovascular diseases. The journal publishes Review Articles, Articles, Correspondence and Comments.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


