A Nomogram for Predicting Cancer-Specific Survival in Young Patients With Advanced Lung Cancer Based on Competing Risk Model
Abstract
Background
Young lung cancer is a rare subgroup accounting for 5% of lung cancer. The aim of this study was to compare the causes of death (COD) among lung cancer patients of different age groups and construct a nomogram to predict cancer-specific survival (CSS) in young patients with advanced stage.
Methods
Lung cancer patients diagnosed between 2004 and 2015 were extracted from the Surveillance, Epidemiology, and End Results (SEER) database and stratified into the young (18–45 years) and old (> 45 years) groups to compare their COD. Young patients diagnosed with advanced stage (IVa and IVb) from 2010 to 2015 were reselected and divided into training and validation cohorts (7:3). Independent prognostic factors were identified through the Fine-Gray's test and further integrated to the competing risk model. The area under the receiver operating characteristic curve (AUC), consistency index (C-index), and calibration curve were applied for validation.
Results
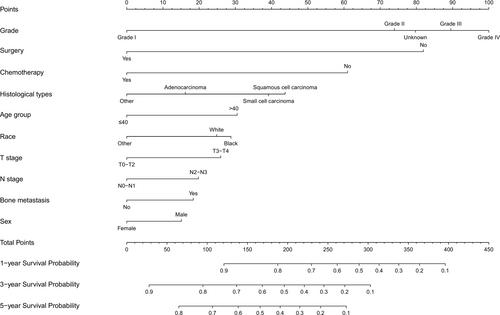
The proportion of cancer-specific death (CSD) in young patients was higher than that in old patients with early-stage lung cancer (p < 0.001), while there was no difference in the advanced stage (p = 0.999). Through univariate and multivariate analysis, 10 variables were identified as independent prognostic factors for CSS. The AUC of the 1-, 3-, and 5-year prediction of CSS was 0.688, 0.706, and 0.791 in the training cohort and 0.747, 0.752, and 0.719 in the validation cohort. The calibration curves demonstrated great accuracy. The C-index of the competing risk model was 0.692 (95% CI: 0.636–0.747) in the young patient cohort.
Conclusion
Young lung cancer is a distinct entity with a different spectrum of competing risk events. The construction of our nomogram can provide new insights into the management of young patients with lung cancer.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


