Cesarean section at full dilatation in the first birth is not associated with an increased risk of subsequent miscarriage: A historical cohort study
Abstract
Introduction
Cesarean section at full dilatation has been associated with an increased risk of subsequent preterm birth. We hypothesized that there may be an increased risk of miscarriage in pregnancies that follow cesarean section at full dilatation. This study aimed to determine if a first-term (≥37 weeks) cesarean section at full dilatation is associated with an increased risk of miscarriage in the next pregnancy.
Material and Methods
A historical cohort study was conducted using routinely collected hospital data within the Aberdeen Maternity and Neonatal Databank (AMND). The population included were women who had a first-term birth and who had a second birth recorded within the AMND. Logistic and multinomial regression was used to determine any association with miscarriage at any gestation and for early (<13 weeks gestation) and late (13–23 + 6 weeks gestation) miscarriage, with cesarean section at full dilatation defined as the exposure. Miscarriage in the second pregnancy (spontaneous loss of intrauterine pregnancy prior to 24 weeks gestation) was the primary outcome.
Results
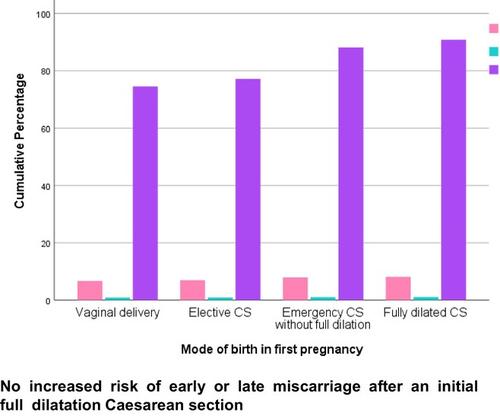
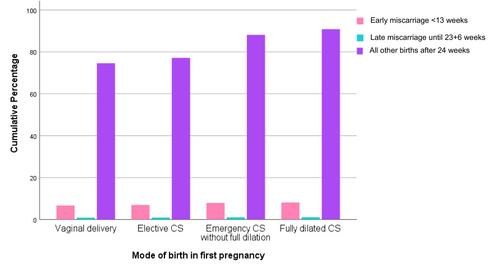
In total, 33 452 women were included. Women who had a first cesarean section at full dilatation were no more likely to have a miscarriage at any gestation than women with all other modes of first birth (including all vaginal births, planned CS, and the first stage of labor (<10 cm dilated CS)) [adjusted OR 0.84 (0.66–1.08); p = 0.18]. There was no association with early or late miscarriage after a CSfd, though the sample size for late miscarriage was small.
Conclusions
This is the first observational study to investigate the risk of miscarriage following first-term CSfd. We found no association between miscarriage at any gestation following a first-term CSfd compared to all other modes of first birth.


 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


