Epidemiology of hypophosphatemia in critical illness: A multicentre, retrospective cohort study
IF 3.7
3区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
Abstract
Introduction
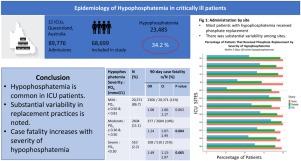
Hypophosphatemia is common in critically ill patients. We have described the epidemiology of hypophosphatemia in patients admitted to the Intensive Care Units.
Methods
A multicentre, retrospective cohort study of 12 ICUs in Queensland, Australia from January 1st, 2015, to December 31st, 2021. Exclusions included readmissions, renal replacement therapy, end-stage renal disease, and palliative intent admissions and transfers from other ICUs. Patients were classified into four groups based on the severity of the first episode of low serum phosphate (PO4): “None” (PO4: ≥0.81 mmol/L, “Mild” (PO4: ≥0.50 & <0.81 mmol/L) “Moderate” (PO4: ≥0.30 & <0.50 mmol/L) and “Severe” (PO4: <0.30 mmol/L). A mixed-effect logistic regression model, including hospital as a random effect, was developed to examine factors associated with 90-day case fatality.
Results
Of the 89,776 patients admitted, 68,699 patients were included in this study, with 23,485 (34.2%) having hypophosphatemia with onset mostly on Day 2 of ICU admission and correcting to normal 3 days after hypophosphatemia was identified. There was substantial variation among participating ICUs in phosphate replacement; the threshold, and the route by which it was replaced. Day-90 case fatality increased with severity of hypophosphatemia (None: 3974 (8.8%), Mild: 2306 (11%), Moderate: 377 (14%); Severe: 108 (21%) (p < 0.001)). Multivariable regression analysis showed that compared to those without hypophosphatemia, patients with moderate (odds ratio (OR) 1.24; 95% confidence intervals (CI) 1.07–1.44; p = 0.004) or severe (OR 1.49; 95% CI 1.13–1.97; p = 0.005) hypophosphatemia had increased risk of 90-day case fatality.
Conclusion
Hypophosphatemia was common, and mostly occurred on day 2 with early correction of serum phosphate. Phosphate replacement practices were variable among ICUs. Moderate and severe hypophosphatemia was associated with increased 90-day case fatality.
危重病人低磷血症的流行病学:一项多中心、回顾性队列研究。
简介低磷酸盐血症在重症患者中很常见。我们描述了重症监护病房住院患者低磷酸盐血症的流行病学:方法:对澳大利亚昆士兰州的 12 个重症监护病房进行多中心、回顾性队列研究,研究时间为 2015 年 1 月 1 日至 2021 年 12 月 31 日。不包括再入院、肾替代治疗、终末期肾病、姑息治疗和从其他重症监护病房转入的患者。根据首次出现低血清磷酸盐(PO4)的严重程度,将患者分为四组:无"(PO4:≥ 0.81 mmol/L)、"轻度"(PO4:≥ 0.50 & < 0.81 mmol/L)、"中度"(PO4:≥ 0.30 & < 0.50 mmol/L)和 "重度"(PO4:< 0.30 mmol/L)。我们建立了一个混合效应逻辑回归模型,将医院作为随机效应,以研究与 90 天病死率相关的因素:在入院的89776名患者中,有68699名患者被纳入本研究,其中有23485名患者(34.2%)出现低磷血症,大多在入住ICU的第2天发病,并在发现低磷血症3天后恢复正常。参与研究的重症监护病房在磷酸盐置换、阈值和置换途径方面存在很大差异。第 90 天的病死率随着低磷酸盐血症严重程度的增加而增加(无:3974 例(8.8%);轻度:2306 例(11%);中度:377 例(14%);重度:377 例(14%)):中度:377 例(14%);重度:108 例(21%):低磷酸盐血症很常见,大多发生在第 2 天,应及早纠正血清磷酸盐。各重症监护病房的磷酸盐替代方法各不相同。中度和重度低磷血症与 90 天病死率增加有关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Anaesthesia Critical Care & Pain Medicine
ANESTHESIOLOGY-
CiteScore
6.70
自引率
5.50%
发文量
150
审稿时长
18 days
期刊介绍:
Anaesthesia, Critical Care & Pain Medicine (formerly Annales Françaises d''Anesthésie et de Réanimation) publishes in English the highest quality original material, both scientific and clinical, on all aspects of anaesthesia, critical care & pain medicine.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


