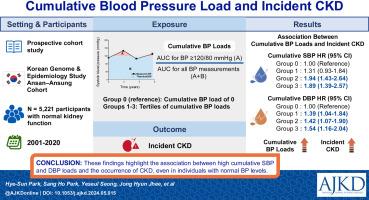
Cumulative Blood Pressure Load and Incident CKD
IF 9.4
1区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Rationale & Objective
The association of long-term cumulative blood pressure (BP) loads with the risk of incident chronic kidney disease (CKD) remains a matter of debate. This study investigated this association among healthy Korean adults with normal kidney function.
Study Design
Prospective cohort study.
Setting & Participants
We analyzed 5,221 participants without CKD in the Korean Genome and Epidemiology Study. Cumulative systolic and diastolic BP (SBP and DBP) loads were calculated as the ratios of the areas under the curve (AUC) for SBP ≥120 mm Hg or ≥80 mm Hg for DBP divided by the AUC for all SBP or DBP measurements during the exposure period. These AUCs were categorized into 4 groups: group 0 (reference), cumulative BP load of 0 and groups 1-3, tertiles of cumulative BP loads.
Outcome
Primary end point was incident CKD defined as a composite of an estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2 or proteinuria greater than 1+ on dipstick examination for at least 2 consecutive measurements ≥90 days apart.
Analytical Approach
Multivariable Cox proportional hazards regression to estimate the independent association of cumulative BP loads with incident CKD.
Results
Higher cumulative SBP and DBP loads were associated with an increased risk of incident CKD (HR, 1.23 [95% CI, 1.12-1.35] for SBP; and HR, 1.14 [95% CI, 1.04-1.26] for DBP loads for each 1.0-unit greater load). Compared with SBP group 0, groups 2 and 3 were associated with 1.94- and 1.89-fold greater risk of incident CKD. Compared with DBP group 0, groups 2 and 3 were associated with 1.42- and 1.54-fold greater risks. These associations of high cumulative BP loads with an increased risk of incident CKD remained consistent even in the subgroups not taking antihypertensive agents or without prior hypertension diagnosis.
Limitations
The assessment of CKD outcomes relied on eGFR and spot urine tests.
Conclusions
These findings highlight the association between high cumulative SBP and DBP loads and the occurrence of CKD, even in individuals with normal BP levels.
Plain-Language Summary
Although hypertension is a major risk factor for chronic kidney disease (CKD), most studies have focused on single-point blood pressure (BP) measurements. To explore the association between long-term cumulative BP load and the development of CKD, 5,221 Korean adults with normal kidney function were included in this study. Cumulative systolic BP and diastolic BP load both exhibited a significant association with an increased risk of incident CKD. Notably, the association of cumulative BP loads with elevated risk of incident CKD was evident also in individuals who were not taking antihypertensive agents or who had no previous history of hypertension. These findings underscore the importance of managing long-term exposure to high BP, even in individuals with normal BP levels.
累积血压负荷与慢性肾脏病发病率。
理由和目标:长期累积血压(BP)负荷与慢性肾脏病(CKD)发病风险的关系仍存在争议。本研究旨在调查肾功能正常的健康韩国成年人的这种关联:前瞻性队列研究:我们分析了韩国基因组与流行病学研究中 5221 名未患 CKD 的参与者。累积收缩压和舒张压(SBP和DBP)负荷的计算方法是:SBP≥120 mmHg或DBP≥80 mmHg时的曲线下面积(AUC)除以暴露期间所有SBP或DBP测量值的AUC之比。这些 AUC 被分为四组:0 组(参考值),累积血压负荷为 0;1-3 组,累积血压负荷的分层:主要终点是突发慢性肾功能衰竭,定义为估计肾小球滤过率(eGFR)低于 60 mL/min/1.73 m2 或至少连续两次测量间隔≥90 天的量尺检查蛋白尿大于 1+ 的综合结果:分析方法:多变量 Cox 比例危险度回归估算累积血压负荷与 CKD 发病的独立关联:结果:累积 SBP 和 DBP 负荷越高,发生 CKD 的风险越高(SBP 负荷每增加 1.0 个单位,危险比 [HR] 为 1.23,95% 置信区间 [CI] 为 1.12-1.35;DBP 负荷每增加 1.0 个单位,危险比 [HR] 为 1.14,95% 置信区间 [CI] 为 1.04-1.26)。与 SBP 0 组相比,2 组和 3 组发生 CKD 的风险分别增加了 1.94 倍和 1.89 倍。与 DBP 0 组相比,第 2 组和第 3 组的风险分别增加了 1.42 倍和 1.54 倍。即使在未服用降压药或之前未确诊高血压的亚组中,高累积血压负荷与发生慢性肾脏病风险增加的关系也是一致的:局限性:对慢性肾脏病结果的评估依赖于电子肾小球滤过率和定点尿检:这些发现强调了高累积 SBP 和 DBP 负荷与发生慢性肾脏病之间的关联,即使是血压水平正常的人也是如此。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
American Journal of Kidney Diseases
医学-泌尿学与肾脏学
CiteScore
20.40
自引率
2.30%
发文量
732
审稿时长
3-8 weeks
期刊介绍:
The American Journal of Kidney Diseases (AJKD), the National Kidney Foundation's official journal, is globally recognized for its leadership in clinical nephrology content. Monthly, AJKD publishes original investigations on kidney diseases, hypertension, dialysis therapies, and kidney transplantation. Rigorous peer-review, statistical scrutiny, and a structured format characterize the publication process. Each issue includes case reports unveiling new diseases and potential therapeutic strategies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


