Linking Invasive and Noninvasive Brain Stimulation in Parkinson's Disease: A Randomized Trial
Abstract
Background
Recent imaging studies identified a brain network associated with clinical improvement following deep brain stimulation (DBS) in Parkinson's disease (PD), the PD response network.
Objectives
This study aimed to assess the impact of neuromodulation on PD motor symptoms by targeting this network noninvasively using multifocal transcranial direct current stimulation (tDCS).
Methods
In a prospective, randomized, double-blinded, crossover trial, 21 PD patients (mean age 59.7 years, mean Hoehn & Yahr [H&Y] 2.4) received multifocal tDCS targeting the a-priori network. Twenty-minute sessions of tDCS and sham were administered on 2 days in randomized order. Movement Disorder Society-Unified Parkinson's Disease Rating Scale—Part III (MDS-UPDRS-III) scores were assessed.
Results
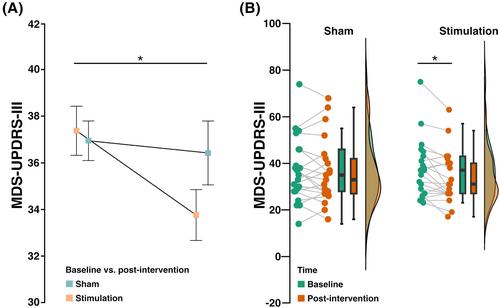
Before intervention, MDS-UPDRS-III scores were comparable in both conditions (stimulation days: 37.38 (standard deviation [SD] = 12.50, confidence interval [CI] = 32.04, 42.73) vs. sham days: 36.95 (SD = 13.94, CI = 30.99, 42.91), P = 0.63). Active stimulation resulted in a reduction by 3.6 points (9.7%) to 33.76 (SD = 11.19, CI = 28.98, 38.55) points, whereas no relevant change was observed after sham stimulation (36.43 [SD = 14.15, CI = 30.38, 42.48], average improvement: 0.5 [1.4%]). Repeated-measures analysis of variance (ANOVA) confirmed significance (main effect of time: F(1,20)=4.35, P < 0.05). Tukey's post hoc tests indicated MDS-UPDRS-III improvement after active stimulation (t [20] = 2.9, P = 0.03) but not after sham (t [20] = 0.42, P > 0.05). In a subset of patients that underwent DBS surgery later, their DBS response correlated with tDCS effects (R = 0.55, P(1) = 0.04).
Conclusion
Noninvasive, multifocal tDCS targeting a DBS-derived network significantly improved PD motor symptoms. Despite a small effect size, this study provides proof of principle for the successful noninvasive neuromodulation of an invasively identified network. Future studies should investigate repeated tDCS sessions and their utility for screening before DBS surgery. © 2024 The Author(s). Movement Disorders published by Wiley Periodicals LLC on behalf of International Parkinson and Movement Disorder Society.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


