Antiviral therapy in cats progressively infected with feline leukaemia virus: lessons from a series of 18 consecutive cases from Australia
Abstract
Background
It is doubtful that any of the treatments proposed for feline leukaemia virus (FeLV) infection are effective, despite the entity being described 60 years ago.
Methods
Eighteen pet cats with progressive FeLV infections were recruited in Australia. One or more antiviral drugs were trialled in 16 cats, while two FeLV-infected cats were not handleable and served as untreated controls. Six cats were administered RetroMAD1™ only (0.5 mg/kg orally twice daily), a commercially available recombinant chimeric protein with proposed antiretroviral activity. Three cats were administered the integrase inhibitor raltegravir only (10–15 mg/kg orally twice daily), a drug used as a component of highly effective antiretroviral therapy for human immunodeficiency virus (HIV-1) infection. Three cats were administered RetroMAD1™ and raltegravir concurrently, and four cats were administered raltegravir and the reverse transcriptase inhibitor zidovudine (AZT, 5 mg/kg orally twice daily) concurrently. FeLV RNA and p27 antigen loads were measured at two timepoints (T1-2 months and T3-5 months) during therapy and compared to baseline (pretreatment) levels, to assess the response to therapy using linear modelling. The median survival time (MST) of the cats from commencement of FeLV treatment to death was also determined and compared between treatments.
Results
The MST for the 16 FeLV-positive cats which received antiviral therapy was 634 days, while the MST from FeLV diagnosis to death for the two untreated control cats was 780 days. In cats treated with RetroMAD1™, FeLV viral load decreased from T0 to T1-2 months (median viral load reduced from 1339 × 106 to 705 × 106 copies/mL plasma; P = 0.012), but MST was reduced compared to cats not given RetroMAD1™ (426 days vs 1006 days; P = 0.049). Cats treated with raltegravir and AZT had no significant changes in FeLV viral load over time, but p27 antigen load was decreased from T0 to T3-5 months in cats treated with raltegravir (median p27 antigen level reduced from 50.2% to 42.7%; P = 0.005). All other results were not significantly affected by the treatment provided.
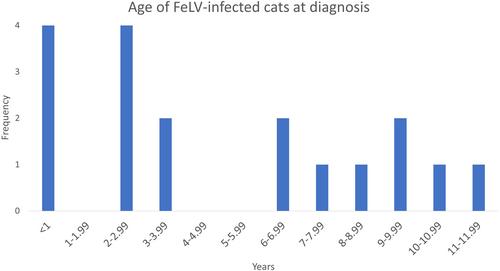
Importantly, statistically significant and substantial associations were found between age at FeLV diagnosis and survival time (P = 0.046, R2 = 18.6) and between FeLV viral load at T0 and survival time (P = 0.004, R2 = 44.4). Younger cats, and cats with higher levels of pretreatment FeLV RNA, had reduced survival times. Cats treated with RetroMAD1™ were typically younger (median age 2.0 vs 8.0 years), likely explaining the observed reduction in MST. A significant association was found between FeLV viral load and p27 antigen load at T0 (P = 0.015, R2 = 32.9).
Conclusions
Results from this small case series do not provide convincing support for the use of RetroMAD1™, raltegravir or AZT, alone or in combination, for the treatment of cats progressively infected with FeLV. The changes observed were biologically insignificant. Age and FeLV viral load at diagnosis are useful prognostic markers, and p27 antigen concentration can be used to predict viral load. Larger field trials should be performed examining antiretroviral therapy in FeLV-positive cats with progressive infections, preferably using three or more drugs from at least two classes, as is standard with human antiretroviral therapy. Future studies would be easier in countries with a higher prevalence of FeLV infections than Australia.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


