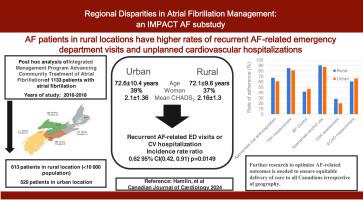
Regional Disparities in Atrial Fibrillation Management: An IMPACT-AF Substudy
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
In rural regions, atrial fibrillation (AF) management is performed predominately by local primary care professionals (PCPs). Prior work has suggested that a disparity in outcomes in AF occurs for those patients living in a rural, vs urban, location.
Methods
This post hoc analysis of the cluster randomized trial Integrated Management Program Advancing Community Treatment of Atrial Fibrillation (IMPACT-AF) compared a clinical decision support system to standard of care. Patients were classified as living in a rural (population < 10,000) or urban location. The outcomes were as follows: AF-related emergency department (ED) visits, unplanned cardiovascular (CV) hospitalizations, AF-related referrals and guideline adherence for AF treatment.
Results
A total of 1133 patients were enrolled from 2016 to 2018; 54.1% (n = 613) were classified as living in a rural location. No differences were present in age (mean, 72 ± 9.63 vs 72.5 ± 10.42 years) or Congestive Heart Failure, Hypertension, Age, Diabetes, Stroke/Transient Ischemic Attack (CHADS2) score (mean, 2.1 ± 1.36 vs 2.16 ± 1.34). Referral rates to general internists were higher in the rural population (13.4% vs 3.9%, P < 0.001), whereas the rate of cardiology referrals was higher in the urban population (10% vs 15%, P = 0.0098). At 12 months, no difference in the composite outcome of AF-related ED visits and CV hospitalizations was seen. Fewer recurrent AF-related ED visits and CV hospitalizations occurred in the urban group (incidence rate ratio [IRR], 0.65 [95% confidence interval (0.44, 0.95), P = 0.0262). The incidence of guideline adherence was similar between the rural (IRR, 3.7 ± 1.2) and urban (IRR, 3.6 ± 1.2; P = 0.11) groups.
Conclusions
AF patients living in rural locations had higher rates of recurrent AF-related ED visits and unplanned CV hospitalizations. Further research to optimize AF-related outcomes is needed to ensure equitable delivery of care to all Canadians, irrespective of geography.
Clinical Trial Registration
NCT01927367.
心房颤动管理中的地区差异:IMPACT 心房颤动子研究
背景在农村地区,心房颤动(AF)的治疗主要由当地的初级保健专业人员(PCP)负责。方法这项群集随机试验 "促进心房颤动社区治疗综合管理计划"(IMPACT-AF)的事后分析比较了临床决策支持系统和标准护理。患者被分为居住在农村(人口< 10,000)和城市两类。结果如下心房颤动相关急诊科(ED)就诊率、非计划性心血管(CV)住院率、心房颤动相关转诊率和心房颤动治疗指南遵守率。结果 2016年至2018年,共有1133名患者入选;54.1%(n = 613)的患者被归类为生活在农村地区。年龄(平均 72 ± 9.63 岁 vs 72.5 ± 10.42 岁)或充血性心力衰竭、高血压、年龄、糖尿病、卒中/短暂性脑缺血发作(CHADS2)评分(平均 2.1 ± 1.36 vs 2.16 ± 1.34)无差异。农村人口的普通内科医生转诊率更高(13.4% vs 3.9%,P < 0.001),而城市人口的心脏病学转诊率更高(10% vs 15%,P = 0.0098)。12 个月后,心房颤动相关急诊就诊和冠心病住院的综合结果无差异。城市组心房颤动相关急诊就诊和冠心病住院的复发率较低(发病率比 [IRR],0.65 [95% 置信区间 (0.44, 0.95),P = 0.0262)。农村组(IRR,3.7 ± 1.2)和城市组(IRR,3.6 ± 1.2;P = 0.11)遵守指南的发生率相似。需要进一步研究如何优化心房颤动相关的结果,以确保为所有加拿大人提供公平的医疗服务,而不论其地理位置如何。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

CJC Open
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
3.30
自引率
0.00%
发文量
143
审稿时长
60 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


