Clinical characteristics, risk factor analysis and peripheral blood cell changes for early warning of multidrug-resistant bacteria (MDR) infection in elderly patients
Abstract
Objective
To explore peripheral blood indicators that may serve as early indicators for multidrug-resistant bacteria (MDR) infections in this demographic, with the goal of providing reference suggestions for the clinical prevention of MDR infections in elderly inpatients.
Methods
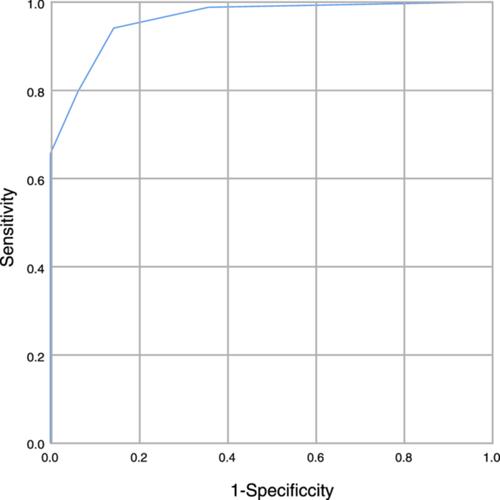
Clinical data of patients were divided into the MDR-infected group (n = 488) and the MDR-uninfected group (n = 233) according to the results of drug sensitivity experiments, risk factors for MDR infection, and peripheral blood indicators related to MDR infections were analyzed using univariate and multivariate logistic regression in conjunction with the construction of a Chi-squared automatic interaction detector (CHAID) decision tree model, considering statistical significance at p < .05.
Results
Of 721 patients, 488 multidrug-resistant strains were identified. Among them, with Staphylococcus spp. the most prevalent in 148 strains. The most frequent detection of MDR occurred in puncture fluid samples (167 cases). Univariate and multivariate regression analyses revealed that prolonged hospitalization, use of antibiotics preadmission, duration of antibiotics, invasive procedures or recent surgery, and coexisting lung disease were independent risk factors for contracting MDR. Subsequent analysis comparing the aforementioned influences with peripheral blood cells revealed associations between the number of antibiotic treatment days and increased neutrophil-to-lymphocyte ratio (NLR), platelet count-to-lymphocyte ratio (PLR), neutrophils, decreased lymphocytes, and increased eosinophils; preadmission antibiotic use correlated with increased PLR, NLR, neutrophils, and decreased lymphocytes; and invasive manipulation or surgery correlated with increased PLR and NLR.
Conclusions
Elevated NLR, PLR, neutrophils, lowered lymphocytes, and eosinophils may serve as early indicators of MDR infections in elderly hospitalized patients.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


