Bowel burdens: a systematic review and meta-analysis examining the relationships between bowel dysfunction and quality of life after spinal cord injury
IF 2.2
4区 医学
Q3 CLINICAL NEUROLOGY
引用次数: 0
Abstract
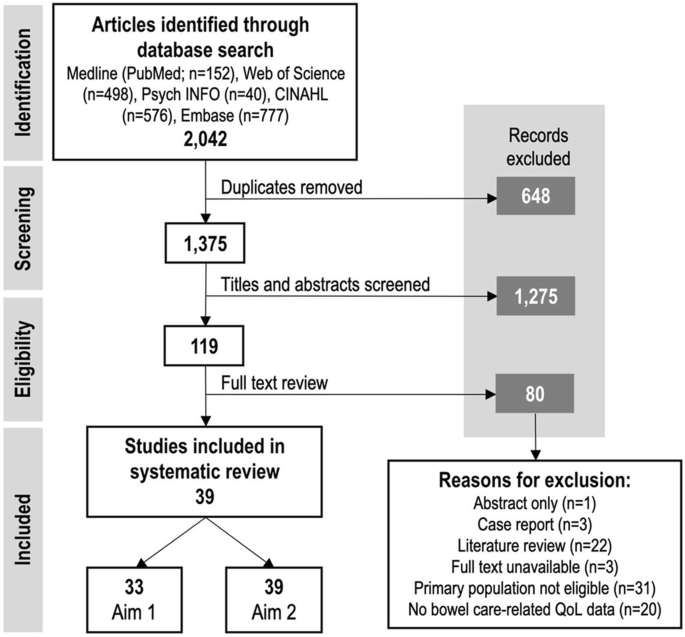
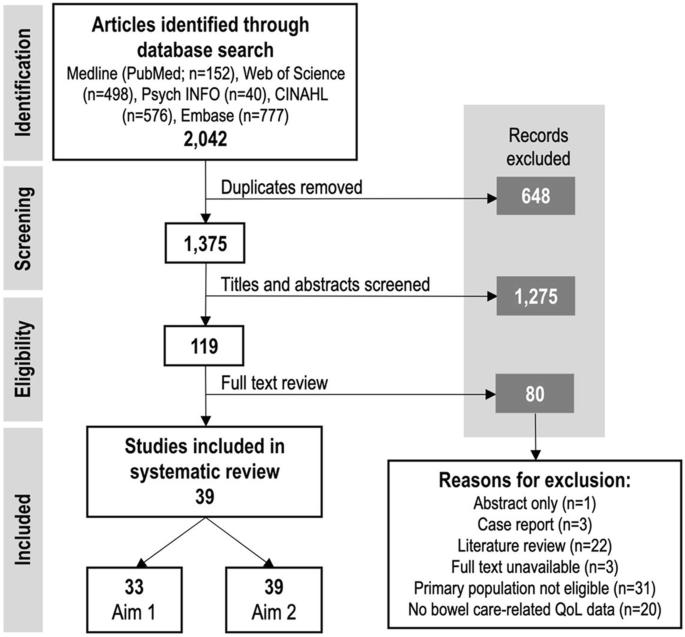
Systematic review and meta-analysis. Many individuals with spinal cord injury (SCI) experience autonomic dysfunction, including profound impairments to bowel and cardiovascular function. Neurogenic bowel dysfunction (NBD) is emerging as a potential determinant of quality of life (QoL) after SCI. For individuals with high-level lesions ( > T6), bowel care-related autonomic dysreflexia (B-AD; profound episodic hypertension) further complicates bowel care. We aimed to evaluate the extent of bowel dysfunction after SCI, and the impact of bowel dysfunction on QoL after SCI. We searched five databases to identify research assessing the influence of NBD or B-AD on QoL after SCI. Metrics of bowel dysfunction (fecal incontinence [FI], constipation, time to complete, and B-AD) and QoL data were extracted and synthesised. Where possible, meta-analyses were performed. Our search identified 2042 titles, of which 39 met our inclusion criteria. Individuals with SCI identified problems with NBD (74.7%), FI (56.9%), and constipation (54.6%), and 49.3% of individuals with SCI > T6 experienced B-AD. Additionally, 40.3% of individuals experienced prolonged defecation ( > 30 min). Moderate/severe deterioration in QoL due to NBD was reported by 55.5% of individuals with SCI, with negative impacts on physical, emotional, and social health-related QoL associated with inflexibility of bowel routines, fear of accidents, and loss of independence. Bowel dysfunction and bowel care challenges are prevalent and disabling for individuals with SCI, with a profoundly negative impact on QoL. Improving bowel management is a key target to improve QoL for those living with SCI.
肠道负担:对脊髓损伤后肠道功能障碍与生活质量之间关系的系统回顾和荟萃分析。
研究设计系统综述和荟萃分析:许多脊髓损伤(SCI)患者会出现自主神经功能障碍,包括肠道和心血管功能严重受损。神经源性肠功能障碍(NBD)正在成为影响 SCI 后生活质量(QoL)的潜在决定因素。对于高位病变(> T6)患者,与肠道护理相关的自主反射障碍(B-AD;极度发作性高血压)使肠道护理更加复杂。我们旨在评估 SCI 后肠道功能障碍的程度以及肠道功能障碍对 SCI 后 QoL 的影响:我们搜索了五个数据库,以确定评估 NBD 或 B-AD 对 SCI 后 QoL 影响的研究。我们提取并综合了肠道功能障碍的指标(大便失禁 [FI]、便秘、排便时间和 B-AD)和 QoL 数据。在可能的情况下,还进行了荟萃分析:我们的搜索发现了 2042 篇论文,其中 39 篇符合我们的纳入标准。SCI患者发现了NBD(74.7%)、FI(56.9%)和便秘(54.6%)等问题,49.3%的SCI > T6患者出现了B-AD。此外,40.3%的患者排便时间过长(> 30 分钟)。55.5%的 SCI 患者表示,排便障碍导致 QoL 中度/严重恶化,对身体、情感和社会健康相关 QoL 造成负面影响,包括排便程序不灵活、害怕发生意外以及丧失独立性:结论:肠道功能障碍和肠道护理方面的挑战对于患有 SCI 的人来说是普遍存在的,而且会造成残疾,对 QoL 产生深远的负面影响。改善肠道管理是提高 SCI 患者 QoL 的关键目标。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Spinal cord
医学-临床神经学
CiteScore
4.50
自引率
9.10%
发文量
142
审稿时长
2 months
期刊介绍:
Spinal Cord is a specialised, international journal that has been publishing spinal cord related manuscripts since 1963. It appears monthly, online and in print, and accepts contributions on spinal cord anatomy, physiology, management of injury and disease, and the quality of life and life circumstances of people with a spinal cord injury. Spinal Cord is multi-disciplinary and publishes contributions across the entire spectrum of research ranging from basic science to applied clinical research. It focuses on high quality original research, systematic reviews and narrative reviews.
Spinal Cord''s sister journal Spinal Cord Series and Cases: Clinical Management in Spinal Cord Disorders publishes high quality case reports, small case series, pilot and retrospective studies perspectives, Pulse survey articles, Point-couterpoint articles, correspondences and book reviews. It specialises in material that addresses all aspects of life for persons with spinal cord injuries or disorders. For more information, please see the aims and scope of Spinal Cord Series and Cases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


