Diabetes misconceptions, seriousness, motivation, self-efficacy and stigma: A cross-sectional comparison of eight Australian diabetes communication campaign videos
Abstract
Aim
This study examines potential intended (attitudes, motivation and self-efficacy) and unintended (stigmatisation of diabetes) consequences of past Australian National Diabetes Week campaign videos. Further, outcomes are compared by the extent to which participants perceived their allocated video as stigmatising diabetes.
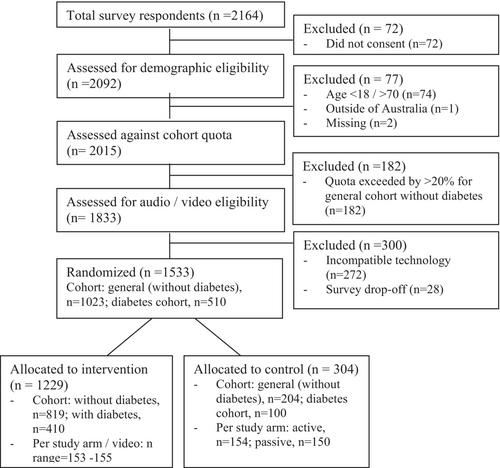
Methods
In this cross-sectional, ten-arm study, participants (adults with or without diabetes; 1:2 ratio) were randomly allocated to view one of eight archival diabetes campaign videos (intervention), or either an active or passive control group. Post-exposure, study-specific scales measured diabetes Misconceptions and Seriousness, General and Diabetes Risk-Reduction Motivation and Self-efficacy, and perceptions of video Stigmatisation of diabetes. Scores were compared by condition (intervention vs. control) and by campaign Stigma (highest vs. lowest tertile score), separately by cohort (with or without diabetes).
Results
The sample included n = 1023 without diabetes; and n = 510 with diabetes (79% type 2 diabetes). No significant differences in outcomes were observed between conditions (intervention vs. control), with one exception: a modest effect on General Self-efficacy among those without diabetes only. Those perceiving high campaign Stigma (15%), relative to low Stigma (60%), reported significantly greater diabetes Misconceptions, lower perceived Seriousness and (among those without diabetes only) lower General Motivation but higher Diabetes Risk Reduction Motivation.
Conclusion
Though limited to a single-exposure, we found little meaningful positive influence of past diabetes campaign videos on diabetes attitudes, behavioural intentions or self-efficacy. Further, campaign videos were perceived as stigmatising by a minority—a potential harmful impact. This novel study has implications for the design, implementation and evaluation of future diabetes campaigns.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


