Comparison of the Burden and Temporal Pattern of Hospitalisations Associated With Respiratory Syncytial Virus (RSV) Before and After COVID-19 in New Zealand
Abstract
Background
Changes in the epidemiology of illnesses caused by respiratory syncytial virus (RSV) infection following the COVID-19 pandemic are reported. The New Zealand (NZ) COVID-19 situation was unique; RSV community transmission was eliminated with the 2020 border closure, with a rapid and large increase in hospitalizations following the relaxation of social isolation measures and the opening of an exclusive border with Australia.
Methods
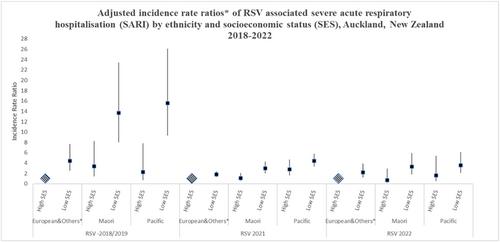
This active population-based surveillance compared the age-specific incidence and seasonality of RSV-associated hospitalizations in Auckland, NZ, for 2 years before and after the 2020 border closures. Hospitalisation rates between years were compared by age, ethnicity (European/other, Māori, Pacific and Asian) and socioeconomic group (1 = least, 5 = most deprived).
Results
There was no RSV transmission in 2020. In all other years, hospitalisation rates were highest for people of Pacific versus other ethnic groups and for people living in the most deprived quintile of households. RSV hospitalisation rates were higher in 2021 and 2022 than in 2018–19. The epidemic peak was higher in 2021, but not 2022, and the duration was shorter than in 2018–19. In 2021, the increase in RSV hospitalisation rates was significant across all age, sex, ethnic and socioeconomic groups. In 2022, the increase in hospitalisation rates was only significant in one age (1– < 3 years), one ethnic (Asian) and one socioeconomic group (quintile 2).
Conclusions
COVID pandemic responses altered RSV-related hospitalisation seasonal patterns. Atypical features of RSV hospitalisation epidemiology were the increase in rates in older children and young adults, which lessened in 2022. Despite these variations, RSV hospitalisations in NZ continue to disproportionately affect individuals of Pacific ethnicity and those living in more socioeconomically deprived households. Whilst future public health strategies focused on RSV disease mitigation need to consider the potential shifts in epidemiological patterns when the transmission is disrupted, these variances must be considered in the context of longer-standing patterns of unequal disease distribution.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


