Combined Mindfulness-Based Stress Reduction and Exercise Intervention for Improving Psychological Well-Being in Patients With Non-Small Cell Lung Cancer
Abstract
Objective
This study aims to assess the clinical effectiveness of combining mindfulness-based stress reduction (MBSR) with exercise intervention in improving anxiety, depression, sleep quality and mood regulation in patients with non-small cell lung cancer (NSCLC).
Methods
A total of 60 patients with NSCLC who had not received surgical treatment were selected using convenience sampling and divided into an intervention group and control group, with 30 patients in each group. The control group received conventional psychological nursing care, whereas the intervention group received a combination of MBwSR and exercise therapy. Before the intervention, a questionnaire was completed to collect the basic data of the two groups. Further questionnaires were administered at 6 and 8 weeks after treatment to assess anxiety, depression, sleep quality and other items included in the five-item Brief Symptom Rating Scale (BSRS-5).
Results
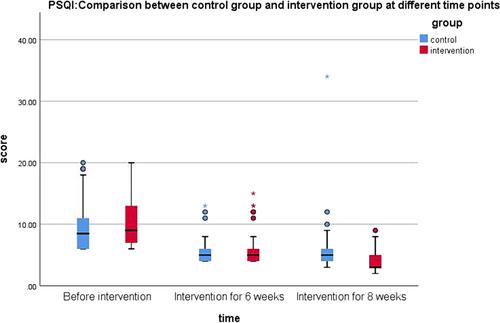
No significant differences between the intervention and control groups were identified in terms of personal and clinical characteristics (p > 0.05). No significant differences were determined in the BSRS-5, Self-Rating Anxiety Scale (SAS), Self-Rating Depression Scale (SDS) or Pittsburgh Sleep Quality Index (PSQI) scores between the intervention and control groups before the intervention. However, 6 and 8 weeks after the intervention, scores were significantly lower in both groups (p < 0.001). Significant differences in the BSRS-5, SAS, SDS and PSQI scores were identified between the two groups at different time points (p < 0.001).
Conclusion
The combination of MBSR and exercise intervention demonstrated improvements in anxiety, depression, sleep quality and BSRS-5 scores in patients with NSCLC.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


