Impact of migraine and fibromyalgia on temporomandibular disorder: A retrospective study on pain, psychological factors and quality of life
Abstract
Objectives
This study assessed the impact of migraine and fibromyalgia (FM) in TMD patients, focusing on pain, anxiety, depression, and quality of life (QoL). Additionally, we investigated how these variables relate to the total number of comorbidities to gain insights into their interactions.
Methods
A retrospective data collection was conducted during January 2016 to December 2022, involving 409 adult TMD patients. TMD patients were categorised into four groups: those without comorbidity (TMD-only) and those with comorbid migraine and/or fibromyalgia (TMD + MG, TMD + FM and TMD + MG + FM). Quantitative variables were compared among them. Linear regression was used to analyse the associations between these variables.
Results
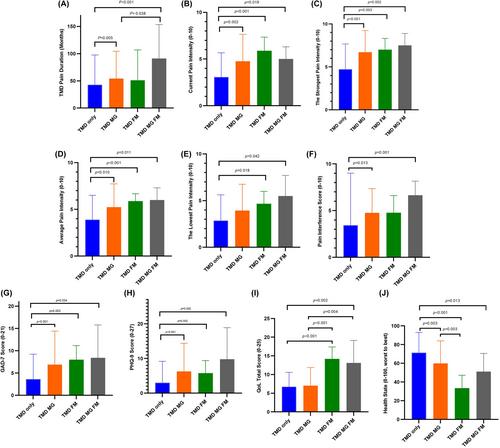
Most of study population were women (79%) with a mean age of 44.43 years. TMD + MG patients reported longer pain duration, higher pain scores and greater pain interference compared with TMD-only patients. Similarly, TMD + FM patients had higher pain intensity than patients with TMD only. Both the TMD + MG and TMD + FM groups had higher levels of anxiety, depression, and health impairment compared with patients with TMD only. Patients with all three pain conditions (TMD + MG + FM) experienced the longest pain duration, highest pain intensity, psychological distress, and impaired QoL. The result showed positive associations between pain outcomes, psychological measures, pain's impact on QoL, and the number of comorbidities and a negative association between overall health states and the number of comorbidities.
Conclusions
These findings underscore the importance of considering the presence of comorbidities and addressing physical and psychological aspects in the management of TMD patients.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


