Engineering photodynamics for treatment, priming and imaging
引用次数: 0
Abstract
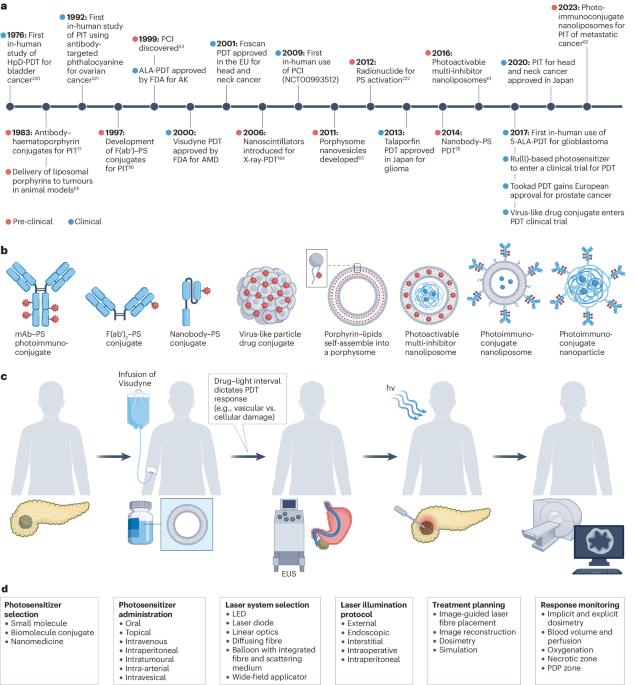
Photodynamic therapy (PDT) is a photochemistry-based treatment approach that relies on the activation of photosensitizers by light to locally generate reactive oxygen species that induce cellular cytotoxicity, in particular for the treatment of tumours. The cytotoxic effects of PDT are depth-limited owing to light penetration limits in tissue. However, photodynamic priming (PDP), which inherently occurs during PDT, can prime the tissue microenvironment to adjuvant therapies beyond the direct PDT ablative zone. In this Review, we discuss the underlying mechanisms of PDT and PDP, and their application to the treatment of cancer, outlining how PDP can permeabilize the tumour vasculature, overcome biological barriers, modulate multidrug resistance, enhance immune responses, increase tumour permeability and enable the photochemical release of drugs. We further examine the molecular engineering of photosensitizers to improve their pharmacodynamic and pharmacokinetic properties, increase their molecular specificity and allow image guidance of PDT, and investigate engineered cellular models for the design and optimization of PDT and PDP. Finally, we discuss alternative activation sources, including ultrasound, X-rays and self-illuminating compounds, and outline key barriers to the clinical translation of PDT and PDP. Photodynamic therapy allows the local destruction of diseased cells and tissues by light. This Review examines how photodynamic therapy and priming can be engineered for the treatment of localized, regional and distant cancer, from photosensitizer engineering to photonic devices and clinical translation.

用于治疗、引导和成像的光动力工程
光动力疗法(PDT)是一种基于光化学的治疗方法,依靠光激活光敏剂在局部产生活性氧,从而诱导细胞毒性,特别是用于治疗肿瘤。由于光在组织中的穿透力有限,光动力疗法的细胞毒性效应受到深度限制。然而,在光动力疗法过程中固有的光动力激发(PDP)可以激发组织微环境,使其成为光动力疗法直接烧蚀区以外的辅助疗法。在这篇综述中,我们将讨论光动力疗法和光动力诱导疗法的基本机制及其在癌症治疗中的应用,概述光动力诱导疗法如何使肿瘤血管通透、克服生物屏障、调节多药耐药性、增强免疫反应、提高肿瘤通透性并使药物的光化学释放成为可能。我们还进一步研究了光敏剂的分子工程学,以改善其药效学和药代动力学特性,提高其分子特异性,实现光动力疗法的图像引导,并研究了用于设计和优化光动力疗法和 PDP 的工程细胞模型。最后,我们讨论了替代激活源,包括超声波、X 射线和自发光化合物,并概述了 PDT 和 PDP 临床转化的主要障碍。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


