The Association Between Late Gadolinium Enhancement by Cardiac Magnetic Resonance and Ventricular Arrhythmia in Patients With Mitral Valve Prolapse: A Systematic Review and Meta-Analysis
Abstract
Introduction
Malignant ventricular arrhythmia (VA) and sudden cardiac death (SCD) have been reported in patients with mitral valve prolapse (MVP); however, effective risk stratification methods are still lacking. Myocardial fibrosis is thought to play an important role in the development of VA; however, observational studies have produced contradictory findings regarding the relationship between VA and late gadolinium enhancement (LGE) in MVP patients. The aim of this meta-analysis and systematic review of observational studies was to investigate the association between left ventricular LGE and VA in patients with MVP.
Methods
We searched the PubMed, Embase, and Web of Science databases from 1993 to 2023 to identify case–control, cross-sectional, and cohort studies that compared the incidence of VA in patients with MVP who had left ventricular LGE and those without left ventricular LGE.
Results
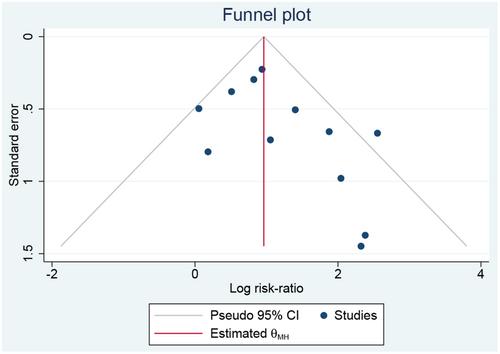
A total of 1464 subjects with MVP from 12 observational studies met the eligibility criteria. Among them, VA episodes were reported in 221 individuals (15.1%). Meta-analysis demonstrated that the presence of left ventricular LGE was significantly associated with an increased risk of VA (pooled risk ratio 2.96, 95% CI: 2.26−3.88, p for heterogeneity = 0.07, I2 = 40%). However, a meta-regression analysis of the prevalence of mitral regurgitation (MR) showed that the severity of MR did not significantly affect the association between the occurrence of LGE and VA (p = 0.079).
Conclusion
The detection of LGE could be helpful for stratifying the risk of VA in patients with MVP.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


