Healthcare professional perspectives on improving inter-pregnancy care after a baby loss for women with type 1 and type 2 diabetes
Abstract
Aims
Women with diabetes (WWD) (type 1 and type 2) are around four times more likely to experience baby loss: miscarriage, stillbirth, neonatal death or termination of pregnancy for medical reasons. Many WWD become pregnant again soon after loss. This study aimed to explore healthcare professional perspectives on improving inter-pregnancy care for WWD after baby loss, as they play a crucial role in facilitating access to support for WWD to prepare for subsequent pregnancy.
Methods
Eighteen healthcare professionals recruited through social media and professional networks between November 2020 and July 2021 participated in a semi-structured remote interview. Data were analysed using thematic analysis.
Results
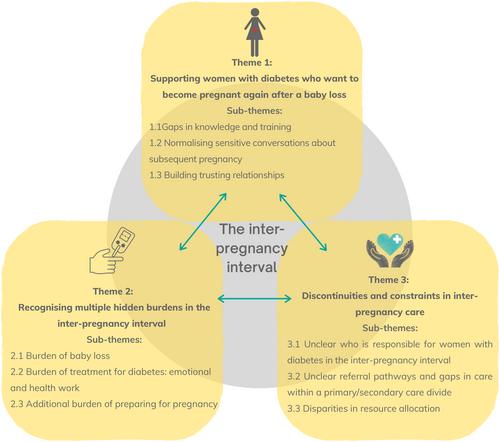
Three main themes were identified: (1) supporting WWD who want to become pregnant again after baby loss; (2) recognising multiple hidden burdens in the inter-pregnancy interval after loss; (3) discontinuities and constraints in inter-pregnancy care. Most participants tended to assume WWD wanted time and space before thinking about pregnancy after loss, so they did not routinely broach the subject. Participants reported receiving little or no training on managing sensitive conversations. Care provision varied across providers, and unclear referral pathways were challenging to navigate. Participants reported concerns that not all healthcare professionals knew how to mitigate pregnancy risks.
Conclusions
It is unclear who is responsible for supporting WWDs preconception health between baby loss and subsequent pregnancy. Healthcare professionals may be reticent to initiate conversations about pregnancy for fear of causing upset or distress. Future research is required to scope out ways to raise awareness among healthcare professionals and practical tips on sensitively raising the topic of subsequent pregnancy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


