A single-site feasibility randomised controlled trial comparing ‘my hypo compass’ short pyscho-educational intervention with standard care alone in individuals with type 1 diabetes and impaired awareness of hypoglycaemia
Abstract
Aims
The HypoCOMPaSS multi-centre trial achieved improvement in hypoglycaemia awareness and 20-fold reduction in severe hypoglycaemia (SH) in a cohort with long-standing type 1 diabetes (T1D). All participants received ‘my hypo compass’ (MHC) brief structured psycho-educational intervention in addition to optimisation of insulin delivery/glucose monitoring. In this 24-week, prospective, single-centre feasibility RCT, we piloted MHC as a sole intervention in comparison to standard clinical care alone (CON).
Methods
Participants with T1D and impaired hypoglycaemia awareness (IAH) (Clarke score ≥4) were recruited. MHC comprised a group/individual 1–2 h face-to-face session followed by a telephone call and second face-to-face session at 4 weeks. Outcome measures at 24 weeks were compared with baseline.
Results
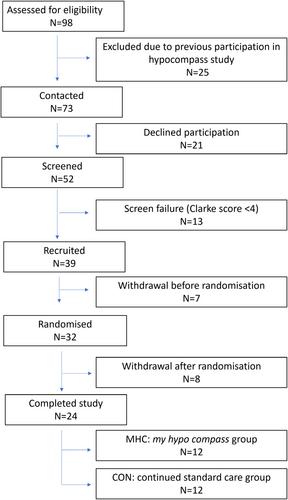
Fifty-two individuals provided consent for screening with 39 fulfilling eligibility criteria. Fifteen withdrew before any study intervention. Twenty-four adults with (mean ± SD) T1D duration 41.0 ± 15.1 years commenced/completed the study (100% visit attendance); 12 randomised to MHC and 12 to CON. All had IAH at baseline and at 24 weeks. Annualised SH rate following MHC was 3.8 ± 19.0 (24 weeks) versus 12.6 ± 3.5 (Baseline) and in CON group 2.0 ± 19.0 (24 weeks) versus 4.6 ± 11.5 (Baseline). ‘Immediate Action’ for and ‘Worry’ about hyperglycaemia measured by the Hyperglycaemia Avoidance Scale appeared lower following MHC. Participants attended all study visits and reflected positively on the MHC intervention.
Conclusions
Feasibility of MHC implementation without additional intervention has been demonstrated. MHC education was associated with positive changes in attitudes and behaviours with the potential to reduce SH risk. MHC provides a validated, simple, well-received programme to fulfil the educational component within RCTs targeting problematic hypoglycaemia and as part of holistic clinical care.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


