Cost-Effectiveness and Budget Impact Analysis of Apixaban and Rivaroxaban Versus Warfarin in the Prevention of Stroke in Patients With Non-Valvular Atrial Fibrillation (NVAF) in Iran
Abstract
Introduction
This study evaluates the cost-effectiveness of Apixaban and Rivaroxaban, compared to Warfarin, for stroke prevention in patients with non-valvular atrial fibrillation in Iran.
Method
A Markov model with a 30-year time horizon was employed to simulate and assess different treatment strategies' cost-effectiveness. The study population comprised Iranian adults with NVAF, identified through specialist consultations, hospital visits, and archival record reviews. Direct medical costs, direct nonmedical, and indirect costs were included. Quality-adjusted life years (QALY) were assessed using an EQ-5D questionnaire. This study utilized a cost-effectiveness threshold of $11 134 per QALY.
Results
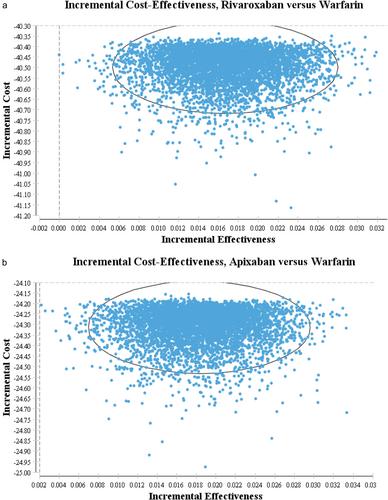
Apixaban demonstrated superior cost-effectiveness compared to Rivaroxaban and Warfarin. Over 30 years, total costs were lower in the Apixaban and Rivaroxaban groups compared to the Warfarin group ($126.18 and $109.99 vs. $150.49). However, Apixaban showed higher total QALYs gained compared to others (0.134 vs. 0.133 and 0.116). The incremental cost-effectiveness ratio for comparing Apixaban to Warfarin was calculated at −1332.83 cost per QALY, below the threshold of $11 134, indicating Apixaban's cost-effectiveness. Sensitivity analyses confirmed the robustness of the findings, with ICER consistently remaining below the threshold. Over 5 years (2024−2028) of Apixaban usage, the incremental cost starts at USD 70 250 296 in the first year and gradually rises to USD 71 770 662 in the fifth year. DSA and PSA were assessed to prove the robustness of the results.
Conclusion
This study shows that Apixaban is a cost-effective option for stroke prevention in non-valvular atrial fibrillation patients in Iran compared to Warfarin.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


