In-Hospital Outcomes and 30-Day Readmission Rate After Transcatheter and Surgical Aortic Valve Replacement in Liver Cirrhosis: A Contemporary Propensity-Matched Analysis
IF 1.4
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Liver cirrhosis is not included in surgical risk prediction models despite being a significant risk factor associated with high periprocedural morbidity and mortality in patients undergoing cardiac surgery. Limited contemporary data exists assessing the outcomes of transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR) in patients with cirrhosis.
Methods
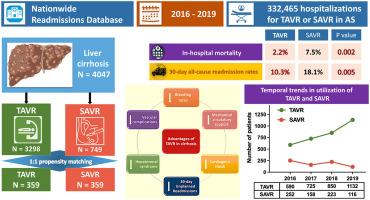
Patients with cirrhosis who underwent TAVR or SAVR were identified from the Nationwide Readmissions Database. Propensity-score matched analysis was performed to compare the clinical characteristics, in-hospital, and 30-day outcomes between the two groups.
Results
Between 2016 and 2019, 4047 patients with cirrhosis underwent TAVR (n = 3298) or SAVR (n = 749). TAVR adoption sharply rose, doubling the number of cases performed during the study period. Following propensity matching among 718 patients, the TAVR group consistently exhibited significantly lower rates of in-hospital mortality (2.2 vs. 7.5%; p = 0.002), bleeding (14.5 vs. 52.9%; p < 0.001), vascular complications (1.4 vs. 5%; p = 0.011), hepatorenal syndrome (3.3 vs. 8.9%; p = 0.003), cardiogenic shock (2.8 vs. 7%; p = 0.015), mechanical circulatory support utilization (0.6 vs. 4.7%; p = 0.001), 30-day all-cause readmission rates (10.3 vs. 18.1%; p = 0.005), and 30-day unplanned readmission rates (10 vs. 16.6%; p = 0.015) compared to the SAVR group. The TAVR group had significantly shorter median hospital stays, lower non-home disposition rates, and reduced hospital costs.
Conclusions
TAVR is associated with significantly lower rates of in-hospital mortality, bleeding, vascular complications, hepatorenal syndrome, cardiogenic shock, mechanical circulatory support utilization, and 30-day readmission rates compared to SAVR and represents a safe therapeutic option for aortic valve replacement in patients with cirrhosis.
肝硬化患者经导管主动脉瓣置换术和外科主动脉瓣置换术后的院内疗效和 30 天再入院率:当代倾向匹配分析
背景肝硬化是心脏手术患者围手术期发病率和死亡率较高的一个重要风险因素,但肝硬化并未被纳入手术风险预测模型。评估肝硬化患者接受经导管主动脉瓣置换术(TAVR)和外科主动脉瓣置换术(SAVR)治疗效果的当代数据有限。结果2016年至2019年间,4047名肝硬化患者接受了TAVR(3298人)或SAVR(749人)。在研究期间,TAVR的采用率急剧上升,手术例数翻了一番。在对 718 名患者进行倾向匹配后,TAVR 组的院内死亡率(2.2 vs. 7.5%;p = 0.002)、出血率(14.5 vs. 52.9%;p < 0.001)、血管并发症(1.4 vs. 5%;p = 0.011)、肝肾综合征(3.3 vs. 8.9%; p = 0.003)、心源性休克(2.8 vs. 7%; p = 0.015)、使用机械循环支持(0.6 vs. 4.7%; p = 0.001)、30 天全因再入院率(10.3 vs. 18.1%; p = 0.005)和 30 天非计划再入院率(10 vs. 16.6%; p = 0.015)。结论与SAVR相比,TAVR的院内死亡率、出血率、血管并发症、肝肾综合征、心源性休克、机械循环支持使用率和30天再入院率均显著降低,是肝硬化患者主动脉瓣置换术的安全治疗选择。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Structural Heart
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
1.60
自引率
0.00%
发文量
81
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


