Platelets in Kawasaki disease: mediators of vascular inflammation
IF 29.4
1区 医学
Q1 RHEUMATOLOGY
引用次数: 0
Abstract
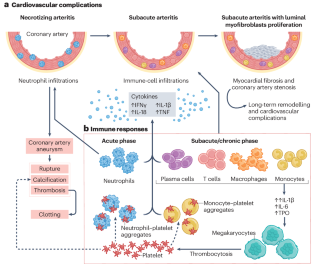
Kawasaki disease, a systemic vasculitis that affects young children and can result in coronary artery aneurysms, is the leading cause of acquired heart disease among children. A hallmark of Kawasaki disease is increased blood platelet counts and platelet activation, which is associated with an increased risk of developing resistance to intravenous immunoglobulin and coronary artery aneurysms. Platelets and their releasate, including granules, microparticles, microRNAs and transcription factors, can influence innate immunity, enhance inflammation and contribute to vascular remodelling. Growing evidence indicates that platelets also interact with immune and non-immune cells to regulate inflammation. Platelets boost NLRP3 inflammasome activation and IL-1β production by human immune cells by releasing soluble mediators. Activated platelets form aggregates with leukocytes, such as monocytes and neutrophils, enhancing numerous functions of these cells and promoting thrombosis and inflammation. Leukocyte–platelet aggregates are increased in children with Kawasaki disease during the acute phase of the disease and can be used as biomarkers for disease severity. Here we review the role of platelets in Kawasaki disease and discuss progress in understanding the immune-effector role of platelets in amplifying inflammation related to Kawasaki disease vasculitis and therapeutic strategies targeting platelets or platelet-derived molecules. This Review outlines the role of platelets in Kawasaki disease and the immune-effector role of platelets in amplifying inflammation related to Kawasaki disease vasculitis and highlights therapeutic strategies that target platelets or platelet-derived molecules.
川崎病中的血小板:血管炎症的介质
川崎病是一种影响幼儿并可导致冠状动脉瘤的全身性血管炎,是儿童后天性心脏病的主要病因。川崎病的一个特征是血小板计数和血小板活化增加,这与对静脉注射免疫球蛋白产生抗药性和冠状动脉瘤的风险增加有关。血小板及其释放物(包括颗粒、微颗粒、微核糖核酸和转录因子)可影响先天免疫、增强炎症反应并促进血管重塑。越来越多的证据表明,血小板还能与免疫细胞和非免疫细胞相互作用,调节炎症。血小板通过释放可溶性介质,促进人体免疫细胞激活 NLRP3 炎症小体和产生 IL-1β。活化的血小板会与单核细胞和中性粒细胞等白细胞形成聚集,增强这些细胞的多种功能,促进血栓形成和炎症。在川崎病急性期,患儿体内的白细胞-血小板聚集增加,可作为疾病严重程度的生物标志物。在此,我们回顾了血小板在川崎病中的作用,并讨论了在了解血小板在放大川崎病血管炎相关炎症中的免疫效应作用方面的进展,以及针对血小板或血小板衍生分子的治疗策略。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Reviews Rheumatology
医学-风湿病学
CiteScore
29.90
自引率
0.90%
发文量
137
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Rheumatology is part of the Nature Reviews portfolio of journals. The journal scope covers the entire spectrum of rheumatology research. We ensure that our articles are accessible to the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


