Diagnosis of acute aortic syndromes with ultrasound and d-dimer: the PROFUNDUS study
IF 5.9
2区 医学
Q1 MEDICINE, GENERAL & INTERNAL
引用次数: 0
Abstract
Background
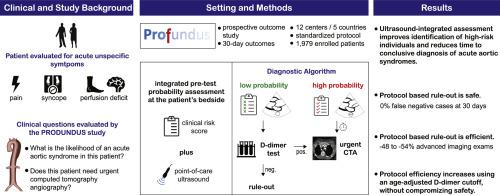
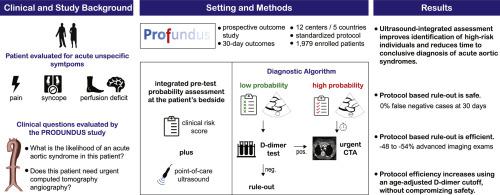
In patients complaining common symptoms such as chest/abdominal/back pain or syncope, acute aortic syndromes (AAS) are rare underlying causes. AAS diagnosis requires urgent advanced aortic imaging (AAI), mostly computed tomography angiography. However, patient selection for AAI poses conflicting risks of misdiagnosis and overtesting.
Objectives
We assessed the safety and efficiency of a diagnostic protocol integrating clinical data with point-of-care ultrasound (POCUS) and d-dimer (single/age-adjusted cutoff), to select patients for AAI.
Methods
This prospective study involved 12 Emergency Departments from 5 countries. POCUS findings were integrated with a guideline-compliant clinical score, to define the integrated pre-test probability (iPTP) of AAS. If iPTP was high, urgent AAI was requested. If iPTP was low and d-dimer was negative, AAS was ruled out. Patients were followed for 30 days, to adjudicate outcomes.
Results
Within 1979 enrolled patients, 176 (9 %) had an AAS. POCUS led to net reclassification improvement of 20 % (24 %/-4 % for events/non-events, P < 0.001) over clinical score alone. Median time to AAS diagnosis was 60 min if POCUS was positive vs 118 if negative (P = 0.042). Within 941 patients satisfying rule-out criteria, the 30-day incidence of AAS was 0 % (95 % CI, 0–0.41 %); without POCUS, 2 AAS were potentially missed. Protocol rule-out efficiency was 48 % (95 % CI, 46–50 %) and AAI was averted in 41 % of patients. Using age-adjusted d-dimer, rule-out efficiency was 54 % (difference 6 %, 95 % CI, 4–9 %, vs standard cutoff).
Conclusions
The integrated algorithm allowed rapid triage of high-probability patients, while providing safe and efficient rule-out of AAS. Age-adjusted d-dimer maximized efficiency.
CLINICAL TRIAL REGISTRATION: Clinicaltrials.gov, NCT04430400
利用超声波和 d-二聚体诊断急性主动脉综合征:PROFUNDUS 研究。
背景:在主诉胸痛、腹痛、背痛或晕厥等常见症状的患者中,急性主动脉综合征(AAS)是罕见的潜在病因。急性主动脉综合征的诊断需要紧急进行先进的主动脉成像(AAI),主要是计算机断层扫描血管造影。然而,选择患者进行 AAI 会带来误诊和过度检查的风险:我们评估了将临床数据与床旁超声(POCUS)和 d-二聚体(单次/年龄调整截止值)相结合的诊断方案的安全性和效率,以选择患者进行 AAI:这项前瞻性研究涉及 5 个国家的 12 个急诊科。POCUS检查结果与符合指南的临床评分相结合,确定了AAS的综合检测前概率(iPTP)。如果 iPTP 较高,则要求进行紧急 AAI。如果 iPTP 较低且 d-二聚体呈阴性,则排除 AAS。对患者进行为期 30 天的随访,以判定结果:结果:1979 名入选患者中,176 人(9%)有 AAS。与单纯的临床评分相比,POCUS的净重新分类率提高了20%(事件/非事件分别为24%/-4%,P<0.001)。如果 POCUS 呈阳性,AAS 诊断的中位时间为 60 分钟;如果呈阴性,则为 118 分钟(P = 0.042)。在符合排除标准的 941 名患者中,AAS 的 30 天发病率为 0 %(95 % CI,0-0.41 %);如果没有 POCUS,可能会漏诊 2 例 AAS。规程排除效率为 48 %(95 % CI,46-50 %),41 % 的患者避免了 AAI。使用年龄调整后的 d-二聚体,排除率为 54%(与标准临界值相比,差异为 6%,95% CI,4%-9%):综合算法可快速分流高概率患者,同时安全有效地排除 AAS。年龄调整后的 d-二聚体能最大限度地提高效率:临床试验注册:Clinicaltrials.gov,NCT04430400。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.60
自引率
6.20%
发文量
364
审稿时长
20 days
期刊介绍:
The European Journal of Internal Medicine serves as the official journal of the European Federation of Internal Medicine and is the primary scientific reference for European academic and non-academic internists. It is dedicated to advancing science and practice in internal medicine across Europe. The journal publishes original articles, editorials, reviews, internal medicine flashcards, and other relevant information in the field. Both translational medicine and clinical studies are emphasized. EJIM aspires to be a leading platform for excellent clinical studies, with a focus on enhancing the quality of healthcare in European hospitals.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


