Beta-cell function and glucose metabolism in patients with chronic pancreatitis
IF 5.9
2区 医学
Q1 MEDICINE, GENERAL & INTERNAL
引用次数: 0
Abstract
Aims
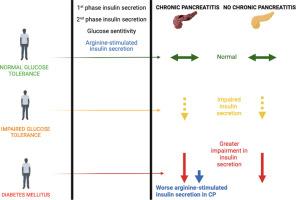
Chronic pancreatitis (CP) is – along with acute pancreatitis - the most frequent cause of diabetes of the exocrine pancreas (DEP). Although insulin deficiency is widely accepted as the major feature of DEP, it is still unclear whether diabetes associated with CP is characterized by additional or different functional defects of the insulin secretory machinery. To identify possible functional defects specifically induced by CP, we performed a cross-sectional study in individuals with normal glucose tolerance (NGT), impaired glucose tolerance (IGT) and diabetes mellitus (DM) comparing patients with and without CP (CP vs. NCP).
Methods
We administered an oral glucose tolerance test (OGTT) to all participants and, according to their glucose tolerance, classified them as NGT, IGT and DM. Insulin sensitivity and beta-cell functional parameters were derived from OGTT, hyperglycemic clamp and hyperinsulinemic euglycemic clamp.
Results
Studying 146 subjects, we found that beta-cell function and insulin secretion were significantly lower in CP compared to NCP patients. However, when we classified the subjects according to OGTT-derived glucose tolerance, we found no differences in beta-cell function or in insulin sensitivity between CP and NCP with the same glucose tolerance status. Of note, we found that arginine-stimulated insulin secretion is reduced only in subjects with CP and DM compared to NCP subjects with DM.
Conclusions
Patients with CP had no specific alterations in insulin secretion and beta-cell function. However, in patients diagnosed with diabetes, we found a lower arginine-stimulated insulin secretion, a marker of reduced functional mass.
慢性胰腺炎患者的β细胞功能和葡萄糖代谢。
目的:慢性胰腺炎(CP)与急性胰腺炎一样,是胰腺外分泌糖尿病(DEP)最常见的病因。尽管胰岛素缺乏被广泛认为是胰腺外分泌糖尿病的主要特征,但与慢性胰腺炎相关的糖尿病是否以胰岛素分泌机制的额外或不同功能缺陷为特征仍不清楚。为了确定 CP 可能诱发的特殊功能缺陷,我们对糖耐量正常(NGT)、糖耐量受损(IGT)和糖尿病(DM)患者进行了一项横断面研究,比较了有 CP 和无 CP 患者(CP vs. NCP):我们对所有参与者进行了口服葡萄糖耐量试验(OGTT),并根据他们的葡萄糖耐量将他们分为 NGT、IGT 和 DM。从 OGTT、高血糖钳夹和高胰岛素血糖钳夹中得出胰岛素敏感性和β细胞功能参数:在对 146 名受试者进行研究后,我们发现 CP 患者的 beta 细胞功能和胰岛素分泌明显低于 NCP 患者。然而,当我们根据 OGTT 导出的葡萄糖耐量对受试者进行分类时,我们发现在葡萄糖耐量状态相同的 CP 和 NCP 之间,β 细胞功能或胰岛素敏感性没有差异。值得注意的是,我们发现与患有 DM 的 NCP 受试者相比,只有患有 CP 和 DM 的受试者精氨酸刺激的胰岛素分泌减少:CP患者的胰岛素分泌和β细胞功能没有特殊改变。然而,在确诊为糖尿病的患者中,我们发现精氨酸刺激的胰岛素分泌较低,而这是功能质量降低的标志。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.60
自引率
6.20%
发文量
364
审稿时长
20 days
期刊介绍:
The European Journal of Internal Medicine serves as the official journal of the European Federation of Internal Medicine and is the primary scientific reference for European academic and non-academic internists. It is dedicated to advancing science and practice in internal medicine across Europe. The journal publishes original articles, editorials, reviews, internal medicine flashcards, and other relevant information in the field. Both translational medicine and clinical studies are emphasized. EJIM aspires to be a leading platform for excellent clinical studies, with a focus on enhancing the quality of healthcare in European hospitals.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


