Brain–computer interfaces for neuropsychiatric disorders
引用次数: 0
Abstract
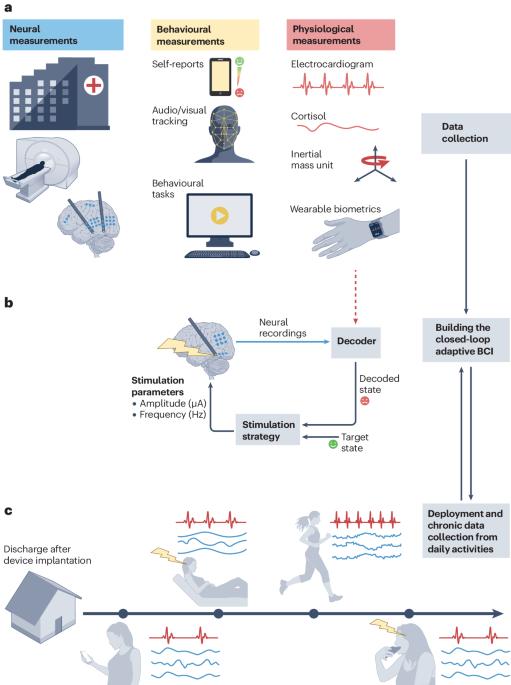
Neuropsychiatric disorders such as major depression are a leading cause of disability worldwide with standard treatments, including psychotherapy or medication, failing many patients. Deep brain stimulation holds great potential as an alternative therapy for treatment-resistant cases; however, improving the efficacy of stimulation therapy for neuropsychiatric disorders is hindered by the complexity as well as inter-individual and intra-individual variability in symptom manifestations, neural representations and response to therapy. These challenges motivate the development of brain–computer interfaces (BCIs) that can decode the symptom state of a patient from brain activity as feedback to personalize the stimulation therapy in closed loop. Here we review progress on developing BCIs for neuropsychiatric care, focusing on neural biomarkers for decoding symptom states, stimulation site selection and closed-loop stimulation strategies. Moreover, we highlight promising data-driven machine learning and system design approaches and provide a roadmap for realizing these BCIs. Finally, we review current limitations, discuss extensions to other treatment modalities and outline the required scientific and technological advances. These advances can enable next-generation BCIs that provide an alternative therapy for treatment-resistant neuropsychiatric disorders. Stimulation therapy for neuropsychiatric disorders is hindered by the complexity and inter-individual and intra-individual variability in symptom manifestations, neural representations and response to therapy. Brain–computer interfaces could model the brain response to stimulation and decode the symptom state of a patient from brain activity as feedback to personalize the stimulation therapy in closed loop.

治疗神经精神疾病的脑机接口
重度抑郁症等神经精神疾病是全球致残的主要原因之一,包括心理治疗或药物治疗在内的标准治疗方法令许多患者望而却步。深部脑刺激作为治疗耐药病例的替代疗法,具有巨大的潜力;然而,由于症状表现、神经表征和治疗反应的复杂性以及个体间和个体内的差异性,提高刺激疗法对神经精神疾病的疗效受到了阻碍。这些挑战推动了脑机接口(BCI)的发展,它可以从大脑活动中解码患者的症状状态,并将其作为闭环刺激疗法个性化的反馈。在此,我们回顾了开发用于神经精神治疗的脑机接口(BCIs)的进展,重点关注用于解码症状状态的神经生物标记物、刺激部位选择和闭环刺激策略。此外,我们还强调了有前景的数据驱动机器学习和系统设计方法,并提供了实现这些 BCI 的路线图。最后,我们回顾了当前的局限性,讨论了向其他治疗模式的扩展,并概述了所需的科学和技术进步。这些进步将使下一代生物识别(BCI)成为治疗耐药性神经精神疾病的替代疗法。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


