Coping with provoked vestibulodynia in a relational context—A cluster analysis of coping patterns and their associations with relational cognitions and goals
Abstract
Background
Provoked vestibulodynia (PVD) is a common pain condition, negatively impacting the relationships and sexual lives of sufferers. Women's coping behaviour has been associated with psychosexual outcomes, yet coping patterns in clinical PVD samples are unexplored, and it is not known how women's coping relates to their relational context.
Method
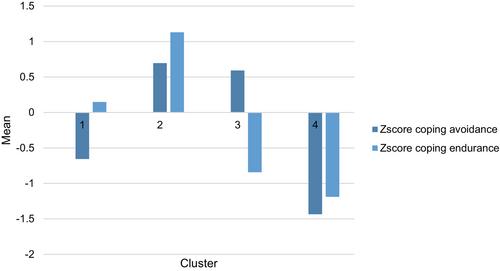
Women (N = 128) with PVD answered questionnaires about psychosexual function, pain coping (avoidance and endurance), relational- and pain catastrophizing, sexual goals and perceived partner responses. Cluster analysis was used to explore coping patterns; clusters were validated on measures of pain and psychosexual function and compared on catastrophizing, sexual goals and partner responses using multivariate analyses of variance.
Results
The analysis yielded four clusters: endurance; combined high avoidance and endurance; avoidance; and combined low. The group with high levels of both avoidance and endurance coping displayed the worst psychosexual outcomes and high levels of pain- and relational catastrophizing, approach and avoidance goals and perceived negative partner responses.
Conclusion
There are distinct patterns of coping among women with PVD, and these coping patterns are associated with psychosexual outcomes and relational cognitions and goals, and perceived partner responses. Women who alternate between avoidance and endurance are more distressed and report worse psychosexual functioning. This pattern needs to be identified and addressed in the treatment of PVD.
Significance Statement
This study extends previous findings on vulvar pain coping patterns to a clinical population of women with PVD. It is further the first study to address the relationship between relational variables, such as partner responses and relational catastrophizing and different coping patterns. Thus, the contribution of this study is the contextualizing of coping patterns among women with PVD. The results showed that a combined pattern of avoidance and endurance coping is associated with high distress, poor psychosexual outcomes, and indications of insufficient relational coping, highlighting the need for clinical assessment and intervention to target both women's individual coping patterns and their relational context.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


