Mother’s own milk and bronchopulmonary dysplasia in appropriate for gestational age preterm infants
IF 3.6
3区 医学
Q2 NUTRITION & DIETETICS
引用次数: 0
Abstract
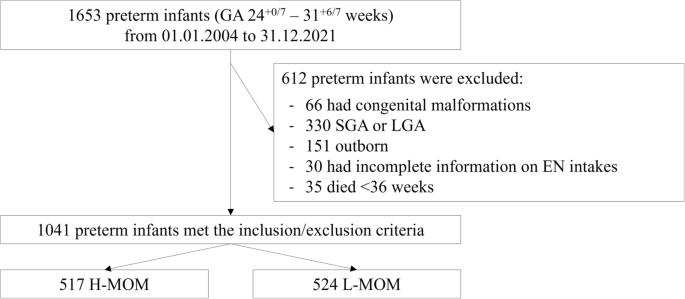
To evaluate the association between mother’s own milk (MOM) and bronchopulmonary dysplasia (BPD) in appropriate for gestational age (AGA) preterm infants <32 weeks. Clinical data of AGA preterm infants (24+0/7–31+6/7 weeks) were reviewed. Infants with ≥66% of cumulative prescribed enteral volumes as MOM from birth to 36 weeks were allocated to the high provision of MOM group (H-MOM), whereas those with <66% were assigned to the low provision of MOM group (L-MOM). Multiple regressions were used to assess the association of H-MOM with BPD and oxygen saturation to fraction inspired oxygen ratio (SFR) at 36 weeks. A total of 1041 infants met the inclusion criteria, with a median provision of cumulative enteral nutrition volumes of 5721 (IQR 2616) mL/kg. Among them, 517 (49.7%) were H-MOM and 524 (50.3%) L-MOM infants. H-MOM showed a reduction in the incidence of BPD to 31.6% compared to L-MOM infants. H-MOM had a lower risk of BPD than L-MOM infants after the adjustment for gestational age, sex, cesarean section, mean SFR at the first hours of life, surfactant administration, patent ductus arteriosus, sepsis, prolonged ventilatory supports/oxygen exposure, and cumulative energy intakes from birth to 36 weeks [aOR: 0.613, p = 0.047]. H-MOM was also associated with a lower risk of SFR in the first quartile at 36 weeks [aOR: 0.616, p = 0.028] than L-MOM. A high provision (≥66%) of enteral volume as MOM from birth to 36 weeks is associated with a reduced risk of both BPD and low SFR at 36 weeks in AGA preterm infants <32 weeks.
适合胎龄早产儿的母乳与支气管肺发育不良。
目的评估适合胎龄(AGA)早产儿的母乳(MOM)与支气管肺发育不良(BPD)之间的关系 方法: 回顾性分析适合胎龄(AGA)早产儿(24+0/7-31+6/7 周)的临床数据:回顾 AGA 早产儿(24+0/7-31+6/7 周)的临床数据。从出生到 36 周期间,肠内 MOM 量累计≥66% 的婴儿被分配到高 MOM 量组(H-MOM),而 MOM 量不足的婴儿则被分配到低 MOM 量组(H-MOM):共有 1041 名婴儿符合纳入标准,累计肠内营养供应量的中位数为 5721(IQR 2616)毫升/千克。其中,517 名(49.7%)为 H-MOM 婴儿,524 名(50.3%)为 L-MOM 婴儿。与 L-MOM 婴儿相比,H-MOM 婴儿的 BPD 发生率降低至 31.6%。在对胎龄、性别、剖宫产、出生后最初几小时的平均 SFR、表面活性物质用量、动脉导管未闭、败血症、长时间通气支持/氧气暴露以及出生至 36 周的累积能量摄入进行调整后,H-MOM 婴儿的 BPD 风险低于 L-MOM 婴儿[aOR:0.613,p = 0.047]。与 L-MOM 相比,H-MOM 也与 36 周时第一四分位数的 SFR 风险较低有关[aOR:0.616,p = 0.028]:结论:在 AGA 早产儿中,从出生到 36 周以 MOM 方式提供大量(≥66%)肠道食物与 36 周时 BPD 和低 SFR 风险的降低有关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
10.60
自引率
2.10%
发文量
189
审稿时长
3-6 weeks
期刊介绍:
The European Journal of Clinical Nutrition (EJCN) is an international, peer-reviewed journal covering all aspects of human and clinical nutrition. The journal welcomes original research, reviews, case reports and brief communications based on clinical, metabolic and epidemiological studies that describe methodologies, mechanisms, associations and benefits of nutritional interventions for clinical disease and health promotion.
Topics of interest include but are not limited to:
Nutrition and Health (including climate and ecological aspects)
Metabolism & Metabolomics
Genomics and personalized strategies in nutrition
Nutrition during the early life cycle
Health issues and nutrition in the elderly
Phenotyping in clinical nutrition
Nutrition in acute and chronic diseases
The double burden of ''malnutrition'': Under-nutrition and Obesity
Prevention of Non Communicable Diseases (NCD)

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


