Tissue changes around dental implants installed in alveolar ridge preservation sites: A 1-year follow-up randomized controlled clinical trial
Abstract
Objective
This study aimed to assess radiographic marginal bone changes 22 months post extraction, which is 1 year after implant loading in alveolar ridge preservation (ARP) sites grafted with a combination of collagen-embedded xenogenic bone substitute (DBBM-C) and collagen matrix (CMX), comparing them with implants placed in naturally healed sites.
Methods
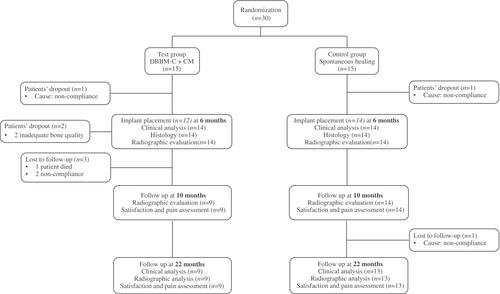
This randomized controlled clinical trial was conducted over 22 months. Patients who needed a single tooth extraction and subsequent implant placement in nonmolar areas were enrolled. The test group received deproteinized bovine bone mineral with 10% collagen covered by a procaine collagen membrane, while the control group allowed spontaneous healing. Radiographic bone level changes were documented using periapical radiographs at implant placement and follow-up visits (6, 10, and 22 months postextraction). Early implant soft tissue exposure, clinical parameters, and patient-reported outcomes were recorded.
Results
Twenty-two out of 28 participants completed a 22-month follow-up, 9 in the test group and 13 in the control group. At 10-month postextraction follow-up, the mean MBL was 1.01 ± 1.04 mm in the treatment group and 0.81 ± 0.93 mm in the control group (p = 0.804). At 22 months, the mean MBL was 2.09 ± 1.03 mm in the treatment group and 1.58 ± 0.73 mm in the control group (p = 0.339). No statistically significant differences in probing depth (PD) and bleeding on probing (BOP) were found at the 22 -month follow-up as well. Soft tissue mean recession was observed in the control group (0.36 ± 0.84 mm), while no recession was found in the test group (p = 0.2). Early implant soft tissue exposure occurred in 33% of test group participants, while none was observed in the control group (p = 0.047).
Conclusion
One year after implant loading, no significant differences in marginal bone resorption were found between implants placed in ARP-treated and naturally healed sites. However, ARP-treated sites exhibited early implant soft-tissue exposure, suggesting a possible impairment in soft tissue healing.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


