Combination of advanced lung cancer inflammation index and nonalcoholic fatty liver disease fibrosis score as a promising marker for surgical procedure selection for hepatocellular carcinoma
Abstract
Aim
Methods of predicting severe postoperative complications after anatomical resection for hepatocellular carcinoma are yet to be established. We aimed to clarify the relationship between inflammation-based prognostic scores and liver fibrosis markers and the incidence of postoperative complications after anatomical resection for hepatocellular carcinoma as well as the usefulness of these markers in surgical procedure selection.
Methods
We included 374 patients with hepatocellular carcinoma who had undergone initial hepatectomy between January 2007 and December 2021. The association between inflammation-based prognostic scores or liver fibrosis markers and postoperative complications was evaluated, and severe postoperative complication rates in the high-risk group defined by these markers were compared in terms of surgical procedure.
Results
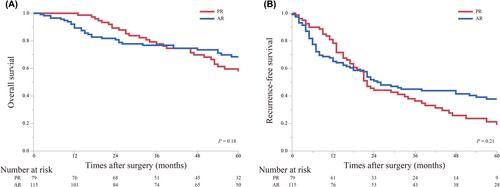
The advanced lung cancer inflammation index and nonalcoholic fatty liver disease fibrosis score correlated significantly with severe postoperative complications after anatomical resection, with areas under the curve of 0.67 and 0.61, respectively. The combined advanced lung cancer inflammation index and nonalcoholic fatty liver disease fibrosis score resulted in a larger area under the curve (0.69). Furthermore, in the high-risk group determined by the combined score, the anatomical resection group had a significantly higher incidence of severe complications than the partial resection group (P < 0.01). There were no significant differences in prognosis among the surgical procedures in the high-risk group.
Conclusion
The combined advanced lung cancer inflammation index and nonalcoholic fatty liver disease fibrosis score serves as a predictive marker for severe postoperative complications after anatomical resection. This combined marker may contribute to appropriate surgical procedure selection.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


