Determining meaningful thresholds for evaluating treatment efficacy in patients with alopecia areata
Abstract
Background
The Severity of Alopecia Tool (SALT) is a clinician-reported outcome measure of scalp hair loss in alopecia areata (AA).
Objectives
To characterise the magnitudes of change in SALT scores corresponding to meaningful treatment benefits from the patient's perspective.
Methods
Anchor-based methods for the estimation of meaningful within-patient change thresholds were applied to pooled data from a randomised, double-blind trial of ritlecitinib. Anchors included a patient-reported measure of change in AA severity, the Patient Global Impression of Change (PGI-C) and three items comprising the Patient Satisfaction with Hair Growth (P-Sat) questionnaire. After reviewing Pearson correlations between change-from-baseline SALT scores and each anchor to confirm adequate association, potential thresholds were computed as mean change-from-baseline SALT scores among patients who reported moderate improvement on the PGI-C and/or moderate satisfaction on each of three P-Sat items at week 24.
Results
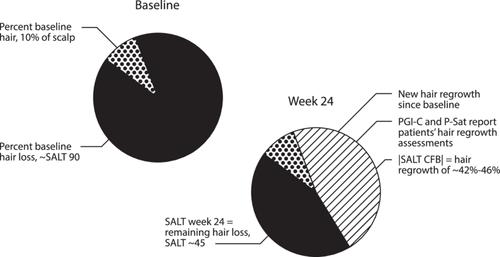
Six hundred and fifty participants (86% adults, 14% adolescents) had mean (standard deviation) SALT scores of 90.6 (14.3) at baseline, suggesting a sample with primarily severe AA. Correlations between SALT change-from-baseline scores and the patient-reported items supported their use as anchors. Estimates based on patients reporting moderate improvement in AA (n = 102) on the PGI-C and those reporting moderate satisfaction on the P-Sat item related to the amount of hair growth at week 24 (n = 122) were −42.2 (26.1) and −43.1 (26.8), respectively. Supportive estimates based on the remaining P-Sat items were similar in magnitude.
Conclusions
Among patients with severe AA, SALT change-from-baseline scores of 42 or 43 represent meaningful improvements. While the achievement of low SALT scores of ≤10–≤20 have been used to characterise efficacy in clinical trials, the amount of change required to meet this endpoint far exceeds the estimates in this study. The treatment goals of individual patients must be considered when evaluating benefit in both clinical trials and clinical practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


