Effect of Implantable Cardioverter-defibrillators in Nonischemic Heart Failure According to Background Medical Therapy: Extended Follow-up of the DANISH Trial
IF 6.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
The Heart Failure Collaboratory (HFC) score integrates types and dosages of guideline-directed pharmacotherapies for heart failure (HF) with reduced ejection fraction (HFrEF). We examined the effects of cardioverter-defibrillator (ICD) implantation according to the modified HFC (mHFC) score in 1116 patients with nonischemic HFrEF from the Danish Study to Assess the Efficacy of ICDs in Patients with Nonischemic Systolic HF on Mortality (DANISH).
Methods and Results
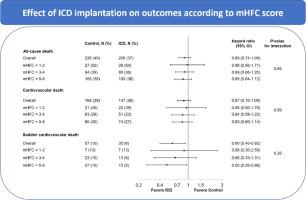
Patients were assigned scores for renin-angiotensin-system inhibitors, beta-blockers and mineralocorticoid receptor antagonists (0, no use; 1, < 50% of maximum dosage; 2, ≥ 50% of maximum dosage). The maximum score was 6, corresponding to ≥ 50% of maximum dosage for all therapies. The median baseline mHFC score was 4, and the median follow-up was 9.5 years. Compared with an mHFC score of 3–4, an mHFC score of 1–2 was associated with a higher rate of all-cause death (mHFC = 1–2: adjusted HR 1.67 [95% CI, 1.23–2.28]; mHFC = 3–4, reference; mHFC = 5–6: adjusted HR 1.07 [95% CI, 0.87–1.31]). ICD implantation did not reduce all-cause death compared with control (reference) (HR 0.89 [95% CI, 0.74–1.08]), regardless of mHFC score (mHFC = 1–2: HR 0.98 [95% CI, 0.56–1.71]; mHFC = 3-4: HR 0.89 [95% CI,0.66–1.20]; mHFC = 5–6: HR 0.85 [95% CI, 0.64–1.12]; Pinteraction, 0.65). Similarly, ICD implantation did not reduce cardiovascular death (HR 0.87 [95% CI, 0.70–1.09]), regardless of mHFC score (Pinteraction, 0.59). The ICD group had a lower rate of sudden cardiovascular death (HR, 0.60 [95% CI,0.40–0.92]); this association was not modified by mHFC score (Pinteraction, 0.35).
Conclusions
Lower mHFC scores were associated with higher rates of all-cause death. ICD implantation did not result in an overall survival benefit in patients with nonischemic HFrEF, regardless of mHFC score.
植入式心律转复除颤器在非缺血性心力衰竭患者中的疗效与背景药物治疗有关:丹麦试验的扩展随访。
背景:心力衰竭协作组(HFC)评分综合了射血分数降低型心力衰竭(HF)指南指导的药物治疗类型和剂量。我们对丹麦评估ICD对非缺血性收缩性心力衰竭患者死亡率疗效的研究(DANISH)中的1116名非缺血性心力衰竭(HFrEF)患者进行了研究,根据修改后的HFC(mHFC)评分考察了植入式心律转复除颤器(ICD)的效果:对患者使用肾素-血管紧张素系统抑制剂、β-受体阻滞剂和矿物质皮质激素受体拮抗剂的情况进行了评分(0:不使用;1:相互作用,0.65)。同样,无论 mHFC 得分如何,植入 ICD 都不会降低心血管疾病的死亡率(HR 0.87 [95%CI,0.70-1.09])(Pinteraction,0.59)。ICD组心血管猝死率较低(HR,0.60 [95% CI,0.40-0.92]);mHFC评分不影响这一关联(Pinteraction,0.35):结论:mHFC评分越低,全因死亡率越高。结论:mHFC 评分越低,全因死亡率越高。无论 mHFC 评分高低,植入 ICD 并未使非缺血性 HFrEF 患者的总生存率获益。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Cardiac Failure
医学-心血管系统
CiteScore
7.80
自引率
8.30%
发文量
653
审稿时长
21 days
期刊介绍:
Journal of Cardiac Failure publishes original, peer-reviewed communications of scientific excellence and review articles on clinical research, basic human studies, animal studies, and bench research with potential clinical applications to heart failure - pathogenesis, etiology, epidemiology, pathophysiological mechanisms, assessment, prevention, and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


