Postoperative radiotherapy versus surgery alone in pN1 oral cavity cancer patients: A meta-analysis
Abstract
Objectives
The aim of this meta-analysis is to evaluate the potential benefits of postoperative radiotherapy (PORT) in patients with pN1 oral cavity squamous cell carcinoma.
Methods
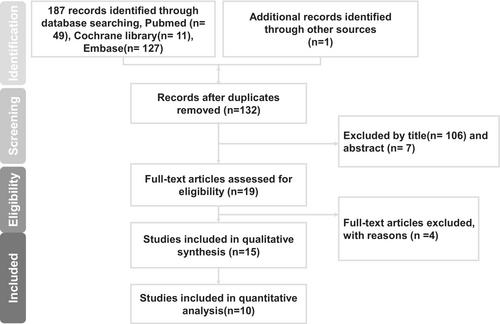
A literature search through major databases was conducted until January 2023. The adjusted hazard ratio (aHR) or risk ratio (RR) with 95% confidence intervals (CIs) of different survival outcomes were extracted and pooled.
Results
Ten studies published between 2005 and 2022, with a pooled patient population of 2888, were included in this meta-analysis. Due to differences in study design and reported outcomes, the studies were categorized into distinct groups. In pN1 patients without extranodal extension (ENE), PORT was associated with a significant improvement in overall survival (OS) (aHR 0.76, 95% CI: 0.61–0.94). In pN1 patients without ENE and positive margins, PORT improved OS (aHR 0.71, 95% CI: 0.56–0.89) and was associated with a lower regional recurrence rate (RR 0.35, 95% CI: 0.15–0.83). However, in pN1 patients without ENE, positive margins, perineural invasion, and lymphovascular invasion, there were no significant differences observed between the PORT and observation groups in either 5-year OS (RR 0.48, 95% CI: 0.07–3.41) or 5-year disease-free survival (RR 0.37, 95% CI: 0.07–2.06).
Conclusions
The current study demonstrated that PORT has the potential to improve OS in pN1 disease. However, the decision of whether to administer PORT still hinges on diverse clinical scenarios, and additional research is necessary to furnish a more conclusive resolution.
Level of Evidence
2.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


