A multi-center, prospective, clinical study to evaluate the anti-reflux efficacy of laparoscopic double-flap technique (lD-FLAP Study)
Abstract
Background
Double-flap technique (DFT) is a reconstruction procedure after proximal gastrectomy (PG). We previously reported a multi-center, retrospective study in which the incidence of reflux esophagitis (RE) (Los Angeles Classification ≥Grade B [LA-B]) 1 year after surgery was 6.0%. There have been many reports, but all of them were retrospective. Thus, a multi-center, prospective study was conducted.
Methods
Laparoscopic PG + DFT was performed for cT1N0 upper gastric cancer patients. The primary endpoint was the incidence of RE (≥LA-B) 1 year after surgery. The planned sample size was 40, based on an estimated incidence of 6.0% and an upper threshold of 20%.
Results
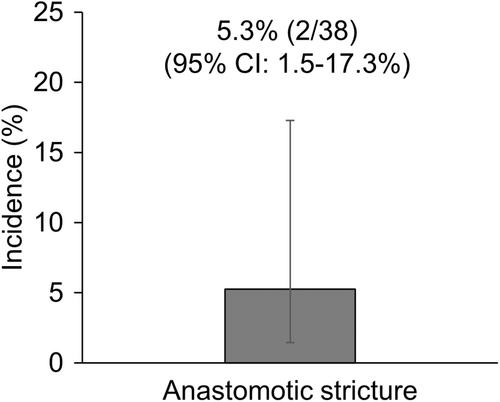
Forty patients were recruited, and 39, excluding one with conversion to total gastrectomy, received protocol treatment. Anastomotic leakage (Clavien–Dindo ≥Grade III) was observed in one patient (2.6%). In 38 patients, excluding one case of postoperative mortality, RE (≥LA-B) was observed in two patients (5.3%) 1 year after surgery, and the upper limit of the 95% confidence interval was 17.3%, lower than the 20% threshold. Anastomotic stricture requiring dilatation was observed in two patients (5.3%). One year after surgery, body weight change was 88.9 ± 7.0%, and PNI <40 and CONUT ≥5, indicating malnutrition, were observed in only one patient (2.6%) each. In the quality of life survey using the PGSAS-45 questionnaire, the esophageal reflux subscale score was 1.4 ± 0.6, significantly better than the public data (2.0 ± 1.0; p = 0.001).
Conclusion
Laparoscopic DFT showed anti-reflux efficacy. Taken together with the acceptable incidence of anastomotic stricture, DFT can be an option for reconstruction procedure after PG.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


