Predictive value of quality of life as measured by KCCQ in heart failure patients: A meta-analysis
Abstract
Background
Studies on the predictive ability of disease-specific health quality of life (QoL) in patients with heart failure (HF) have produced conflicting results. To address these gaps in knowledge, we conducted a meta-analysis to evaluate the predictive value of QoL measured by the Kansas City Cardiomyopathy Questionnaire (KCCQ) in patients with HF.
Materials and Methods
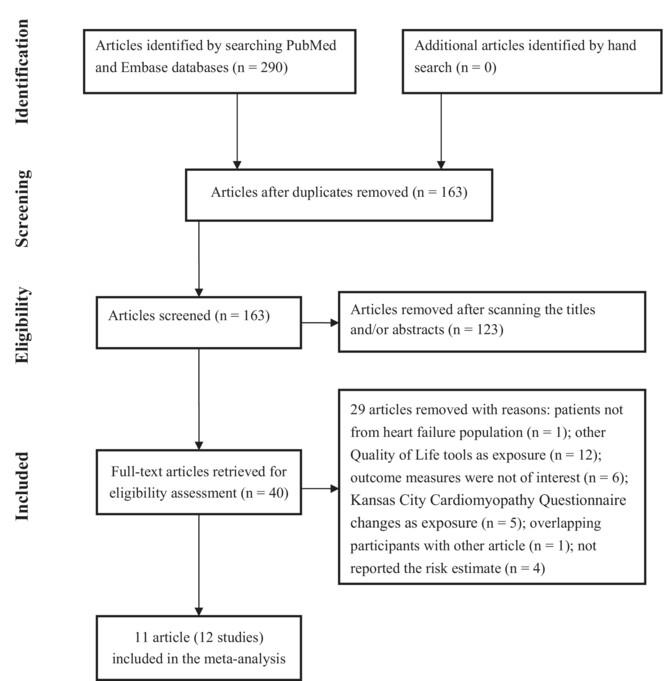
We searched PubMed, and Embase databases to identify studies investigating the predictive utility of baseline QoL measured by the KCCQ in HF patients. The outcome measures were all-cause mortality and HF hospitalisation. The predictive value of QoL was expressed by pooling the adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for the bottom versus the top category of KCCQ score or for per 10-point KCCQ score decrease.
Results
Twelve studies reporting on 11 articles with a total of 34,927 HF patients were identified. Comparison of the bottom with the top KCCQ score, the pooled adjusted HR was 2.34 (95% CI 2.10–2.60) and 2.53 (95% CI 2.23–2.88) for all-cause mortality and HF hospitalisation, respectively. Additionally, a 10-point decrease in KCCQ score was associated with a 12% (95% CI 7%–16%) increased risk of all-cause mortality and a 14% (95% CI 13%–15%) increased risk of HF hospitalisation.
Conclusions
Poor health-related QoL as determined by the lower KCCQ score, was associated with an increased risk of all-cause mortality and HF hospitalisation in patients with HF. Measuring disease-specific health-related QoL using the KCCQ score may provide valuable predictive information for HF patients.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


