Hepatic signal transducer and activator of transcription-3 signalling drives early-stage pancreatic cancer cachexia via suppressed ketogenesis
Abstract
Background
Patients with pancreatic ductal adenocarcinoma (PDAC) often suffer from cachexia, a wasting syndrome that significantly reduces both quality of life and survival. Although advanced cachexia is associated with inflammatory signalling and elevated muscle catabolism, the early events driving wasting are poorly defined. During periods of nutritional scarcity, the body relies on hepatic ketogenesis to generate ketone bodies, and lipid metabolism via ketogenesis is thought to protect muscle from catabolizing during nutritional scarcity.
Methods
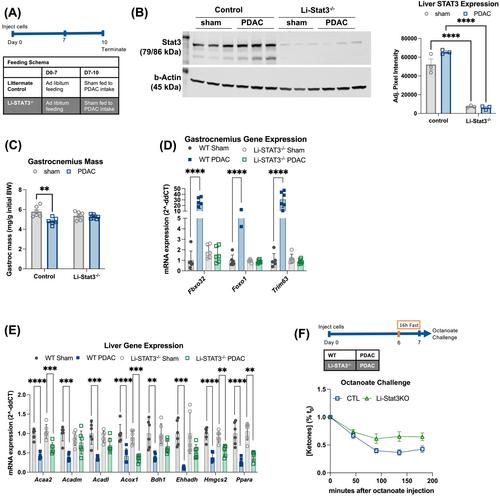
We developed an orthotopic mouse model of early PDAC cachexia in 12-week-old C57BL/6J mice. Murine pancreatic cancer cells (KPC) were orthotopically implanted into the pancreas of wild-type, IL-6−/−, and hepatocyte STAT3−/− male and female mice. Mice were subject to fasting, 50% food restriction, ad libitum feeding or ketogenic diet interventions. We measured longitudinal body composition by EchoMRI, body mass and food intake. At the endpoint, we measured tissue mass, tissue gene expression by quantitative real-time polymerase chain reaction, whole-body calorimetry, circulating hormone levels, faecal protein and lipid content, hepatic lipid content and ketogenic response to medium-chain fatty acid bolus. We assessed muscle atrophy in vivo and C2C12 myotube atrophy in vitro.
Results
Pre-cachectic PDAC mice did not preserve gastrocnemius muscle mass during 3-day food restriction (−13.1 ± 7.7% relative to food-restricted sham, P = 0.0117) and displayed impaired fatty acid oxidation during fasting, resulting in a hypoketotic state (ketogenic response to octanoate bolus, −83.0 ± 17.3%, P = 0.0328; Hmgcs2 expression, −28.3 ± 7.6%, P = 0.0004). PDAC human patients display impaired fasting ketones (−46.9 ± 7.1%, P < 0.0001) and elevated circulating interleukin-6 (IL-6) (12.4 ± 16.5-fold increase, P = 0.0001). IL-6−/− PDAC mice had improved muscle mass (+35.0 ± 3.9%, P = 0.0031) and ketogenic response (+129.4 ± 44.4%, P = 0.0033) relative to wild-type PDAC mice. Hepatocyte-specific signal transducer and activator of transcription 3 (STAT3) deletion prevented muscle loss (+9.3 ± 4.0%, P = 0.009) and improved fasting ketone levels (+52.0 ± 43.3%, P = 0.018) in PDAC mice. Without affecting tumour growth, a carbohydrate-free diet improved tibialis anterior myofibre diameter (+16.5 ± 3.5%, P = 0.0089), circulating ketone bodies (+333.0 ± 117.6%, P < 0.0001) and Hmgcs2 expression (+106.5 ± 36.1%, P < 0.0001) in PDAC mice. Ketone supplementation protected muscle against PDAC-induced atrophy in vitro (+111.0 ± 17.6%, P < 0.0001 myofibre diameter).
Conclusions
In early PDAC cachexia, muscle vulnerability to wasting is dependent on inflammation-driven metabolic reprogramming in the liver. PDAC suppresses lipid β-oxidation and impairs ketogenesis in the liver, which is reversed in genetically modified mouse models deficient in IL-6/STAT3 signalling or through ketogenic diet supplementation. This work establishes a direct link between skeletal muscle homeostasis and hepatic metabolism. Dietary and anti-inflammatory interventions that restore ketogenesis may be a viable preventative approach for pre-cachectic patients with pancreatic cancer.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


